Published: December 2013
Please note that this information will be reviewed every 3 years after publication.
This information is for you if you would like to find out more about cervical smears in pregnancy.
This information may also be helpful if you are a partner, relative or friend of someone who is in this situation.
In the UK, cervical cancer is very rare. To reduce the risk of developing cancer even further, women are offered regular testing to detect changes in the cervix (neck of the womb) at a stage before they become cancerous. The sample that is taken from the cervix is known as a smear test. If your smear test is abnormal, you may be referred for an investigation called a colposcopy, which is a more detailed look at the cervix.
Most women in the UK start having smears by the age of 25. Therefore it is not unusual to be called for a smear test or to be asked to attend colposcopy during pregnancy.
The information here aims to help you better understand your health and your options for treatment and care. Your healthcare team is there to support you in making decisions that are right for you. They can help by discussing your situation with you and answering your questions.
This information is for you if:
- You’re unsure whether you should have your smear or attend colposcopy while you’re pregnant
- You’ve had an abnormal smear result and then discovered you’re pregnant
- You’ve had treatment in the past for an abnormal smear, and are pregnant or are considering having a baby
Within this information, we may use the terms ‘woman’ and ‘women’. However, it is not only people who identify as women who may want to access this information. Your care should be personalised, inclusive and sensitive to your needs, whatever your gender identity.
A glossary of medical terms is available at A-Z of medical terms.
- If you are asked to come for a routine smear test while you are pregnant, you should put it off until after your baby is born. You should let your GP know you have delayed the test so that you can be invited again. This appointment will usually be 3 months after your baby is due.
- If it is not a routine smear, but a repeat smear after a previous abnormality, that you have been called for during pregnancy, then you should still have your smear during pregnancy. The best time to have it done is between 3 and 6 months of pregnancy.
The following information is a guide to whether you should still attend colposcopy even if you are pregnant. Often colposcopy can be postponed until after your baby is born, but in some circumstances you should still attend.
If you are not sure whether you need to attend colposcopy, contact your clinic and they will advise you what to do.
You may be in one of the following situations:
- I have had an abnormal smear. Sometimes women become pregnant in between having their smear test and finding out the results. If colposcopy has been recommended, it is important that you still attend your appointment even though you are pregnant. Colposcopy will not harm your baby and can provide valuable and reassuring information.
- I am being monitored at colposcopy for a mildly abnormal smear. I am due for my follow-up appointment, but I am now pregnant. What should I do? A mildly abnormal smear is likely to get better by itself and you may be being monitored just to make sure all is well. If this is the case, you should notify your colposcopy clinic and you will be given an appointment for 3 months after your baby has been born.
- I have had treatment for an abnormal smear. I am due for my follow-up appointment but I am now pregnant. What should I do? Your follow-up at colposcopy can usually wait until after you have had your baby if:
- this will be your first follow-up appointment and your original treatment was for a mild abnormality called CIN 1
- this will be your first follow-up appointment, your original treatment was for a more severe abnormality called CIN 2 or CIN 3 and your doctor was sure all the abnormal areas were treated
- this is any time after your first follow-up appointment, so long as you have not missed any appointments and your smear tests are up to date and normal.
There are two circumstances, however, where you should still attend for review, even if you are pregnant:
- if your original treatment was for an abnormality called cGIN
- if you had the abnormality called CIN 2 or CIN 3 but your doctor was not sure whether all the abnormal cells were removed.
If you are unsure about your treatment, contact your colposcopy clinic/GP who will have the appropriate information on record and will be able to advise you on what to do.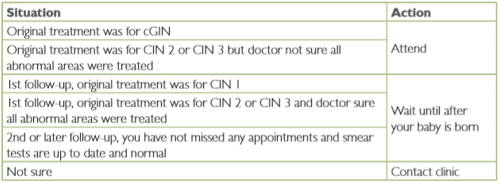
- I have had some bleeding in pregnancy and examination of my cervix suggests that there may be an abnormality present. If you have been referred to colposcopy in this situation, it is very important that you attend
If you have missed some of your appointments, your doctor may advise you to have your smear done or to attend colposcopy even though you are pregnant. The advice you will receive will depend on your individual circumstances.
Sometimes you may need to have a colposcopy repeated. This might be because your first examination was very early in your pregnancy, or if things change, for example if you start bleeding or if you have an offensive-smelling discharge from your vagina.
If you have colposcopy while you are pregnant you will usually need to have a follow-up appointment. This usually takes place about 3 months after your baby is born, so that any further treatment needed can be carried out.
You are more likely to bleed if you have a biopsy or treatment when you are pregnant. Because of this, biopsies and treatment of mild abnormalities can usually be delayed until after your baby is born. If the nurse or doctor does recommend a biopsy while you are pregnant, they will discuss this with you.
This depends on the type of treatment that you have had:
- Sometimes a tiny sample called a punch biopsy is taken for testing from the cervix during colposcopy. Depending on the results, you may need treatment to destroy any abnormal cells. This can be done by heat treatment, laser or freezing. None of these treatments appear to cause any problems in pregnancy.
- Excisional biopsy is where a piece of tissue is removed from the centre of your cervix with the aim of removing all the abnormal cells. Having this type of biopsy is known to be associated with a small increase in the risk of having a baby prematurely. The risk is higher if you have had more than one excisional biopsy or if a large amount of cervix was removed. The exact reason for this risk is not known, but is likely to be due to the amount of tissue removed.
The majority of women who have had treatment to the cervix will have a successful pregnancy and deliver a healthy baby at the normal time.
Because of the small increase in the risk of your baby being born prematurely associated with an excisional biopsy, you may be offered vaginal scans in pregnancy to measure the length of your cervix. This is particularly the case if you have had more than one treatment or if a large amount of your cervix was removed. If you have had a baby born prematurely or a late miscarriage in the past and your cervix appears shortened on the scan, you may be offered to have a stitch put around it to prevent it opening early.
If you are unsure what type of treatment you have had, contact your colposcopy unit. They should be able to tell you what type of biopsy/treatment you have had and how much tissue was removed.
If you need treatment, it is important that you tell the doctor/nurse treating you about your plans. Your doctor will make sure you get the care you need while keeping any risk to any future pregnancies to a minimum. This may mean doing less treatment initially, until your pregnancy is over, and then completing your treatment after your baby is born.
Sources and acknowledgements
This information has been developed by the RCOG Patient Information Committee. It is based on the British Society for Colposcopy and Cervical Pathology (BSCCP) NHS Guidelines for Colposcopy and Programme Management published by the Cancer Screening Programmes (www.cancerscreening.nhs.uk/cervical) and on the RCOG Scientific Impact Paper Obstetric Impact of Treatment for Cervical Intraepithelial Neoplasia (June 2010) produced by the Scientific Advisory Committee. The latter contains a full list of the sources of evidence we have used.
This information has been reviewed before publication by women attending clinics in Warwick, Lancashire and Coleraine.
