Published: June 2015
Please note that this information will be reviewed every 3 years after publication.
Updated: February 2022
To access this leaflet in additional languages, please visit our Translations page.
This information is for you if you want to know more about polycystic ovary syndrome (PCOS).
It may be helpful if you are a partner, relative or friend of someone has PCOS.
The information here aims to help you better understand your health and your options for treatment and care. Your healthcare team is there to support you in making decisions that are right for you. They can help by discussing your situation with you and answering your questions.
This information covers:
- Symptoms of PCOS
- Causes of PCOS
- How PCOS is diagnosed
- What PCOS could mean for your long-term health
- How to reduce long-term health risks
Within this information, we may use the terms ‘woman’ and ‘women’. However, it is not only people who identify as women who may want to access this information. Your care should be personalised, inclusive and sensitive to your needs, whatever your gender identity.
A glossary of medical terms is available at A-Z of medical terms.
Key Points
- Polycystic Ovary syndrome (PCOS) is a common condition in which a hormone imbalance causes irregular periods, increased hair and acne and may affect fertility.
- PCOS is associated with obesity and increased insulin resistance and therefore increases the risk of developing diabetes, heart disease and other conditions later in life.
- Women with PCOS can reduce the risk of long term health problems by having a healthy lifestyle and maintaining normal body weight.
PCOS is a condition that can affect your periods, fertility, hormones and aspects of your appearance. It can also affect your long-term health. Estimates of how many women it affects vary widely from 2 to 26 in every 100 women. This information is about the effects on your long-term health and does not cover specific treatment options for PCOS.
Polycystic ovaries are slightly larger than normal ovaries and have twice the number of follicles (fluid-filled spaces within the ovary that release the eggs when you ovulate).
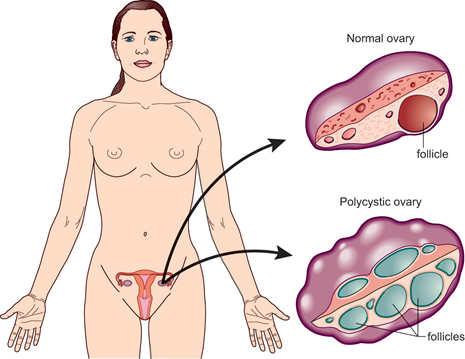
Having polycystic ovaries on an ultrasound does not necessarily mean that you have PCOS. Women with PCOS have symptoms as well as polycystic ovaries.
The symptoms of PCOS include:
- irregular periods or no periods at all
- an increase in facial or body hair (hirsutism)
- loss of hair on your head
- being overweight, experiencing a rapid increase in weight or having difficulty losing weight
- oily skin, acne
- difficulty becoming pregnant (reduced fertility).
Depression and psychological problems can also result from having PCOS.
The symptoms vary from woman to woman. Some women have very few mild symptoms, while others are affected more severely by a wider range of symptoms.
PCOS is a cause of fertility problems in women. For further information see Fertility: Assessment and Treatment for People with Fertility Problems, which is produced by the National Institute for Health and Care Excellence (NICE).
You may still become pregnant even if you do not have periods. If you do not want to become pregnant, you should seek advice from your GP about contraception.
The cause of PCOS is not yet known but it sometimes runs in families. If any of your relatives (mother, aunts, sisters) are affected with PCOS, your risk of developing PCOS may be increased.
The symptoms are related to abnormal hormone levels:
- Testosterone is a hormone that is produced in small amounts by the ovaries in all women. Women with PCOS have slightly higher than normal levels of testosterone and this is associated with many of the symptoms of the condition.
- Insulin is a hormone that controls the level of glucose (a type of sugar) in the blood. If you have PCOS, your body may not respond to insulin (this is known as insulin resistance), so the level of glucose is higher. To try to prevent the glucose levels becoming higher, your body produces even more insulin. High levels of insulin can lead to weight gain, irregular periods, fertility problems and higher levels of testosterone.
Having polycystic ovaries does not mean you have PCOS.
Women with PCOS often have symptoms that come and go, particularly if their weight goes up and down. This can make it a difficult condition to diagnose, which means it may take a while to get a diagnosis.
A diagnosis is made when you have any two of the following:
- irregular, infrequent periods or no periods at all
- an increase in facial or body hair and/or blood tests that show higher testosterone levels than normal
- an ultrasound scan that shows polycystic ovaries.
When a diagnosis is made, you may be referred to a gynaecologist (a doctor who specialises in caring for a woman’s reproductive system) or an endocrinologist (a doctor who specialises in the hormonal system).
If you have PCOS, you are at greater risk of developing the long-term health problems discussed below.
Insulin resistance and diabetes
If your blood glucose does not stay normal, this can lead to diabetes. One or two in every ten women with PCOS go on to develop diabetes at some point. If the diabetes is untreated, this can cause damage to organs in the body. You are also at higher risk of developing diabetes in pregnancy and will e offered a blood test between 24 and 28 weeks for this. Please see RCOG patient information on Gestational diabetes.
If you have PCOS, your risk of developing diabetes is increased further if you:
- are over 40 years of age
- have relatives with diabetes
- developed diabetes during a pregnancy (known as gestational diabetes)
- are obese (a body mass index (BMI) of over 30).
If you are diagnosed with diabetes, you will be given advice about your diet and may be prescribed tablets or insulin injections.
High blood pressure and heart disease
Women with PCOS tend to have high blood pressure, which is likely to be related to insulin resistance and to being overweight rather than to the PCOS itself. High blood pressure can lead to heart problems and should be treated.
Cancer
If you have fewer than three periods a year, the lining of the womb (endometrium) can thicken and this may lead to endometrial cancer in a small number of women.
There are various ways to protect the lining of the womb using the hormone progestogen. Your doctor will discuss the options with you. This may include a five-day course of progestogen tablets used every three or four months, taking a contraceptive pill or using the intrauterine contraceptive system (Mirena®). The options will depend on whether you are trying for a baby.
PCOS does not increase your chance of breast or ovarian cancer.
Depression and mood swings
The symptoms of PCOS may affect how you see yourself and how you think others see you. It can lower your self-esteem.
Snoring and daytime drowsiness
PCOS can lead to fatigue or sleepiness during the day. It is also associated with snoring.
Have a healthy lifestyle
The main ways to reduce your overall risk of long-term health problems are to:
- eat a healthy balanced diet. This should include fruit and vegetables and whole foods (such as wholemeal bread, whole-grain cereals, brown rice and whole-wheat pasta), lean meat, fish and chicken. You should cut down the amount of sugar, salt and caffeine that you eat and drink.
- eat meals regularly, especially breakfast
- take exercise regularly (30 minutes at least three times a week).
Your GP or practice nurse can provide you with full information on eating a healthy diet and exercise.
You should aim to keep your weight to a level that is normal. BMI is the measurement of weight in relation to height and you should aim to keep your BMI between 19 and 25. The NHS website has a BMI calculator.
If you are overweight, it would be helpful to lose weight and maintain your weight at this new level. If your BMI is more than 30, discuss ways of losing weight, including weight-reducing drugs, with your GP, practice nurse or pharmacist.
The benefits of losing weight include:
- a lower risk of insulin resistance and developing diabetes
- a lower risk of heart problems
- a lower risk of cancer of the womb
- more regular periods
- an increased chance of becoming pregnant
- a reduction in acne and a decrease in excess hair growth over time
- improved mood and self-esteem.
You only have to lose a small amount of weight to make a difference to your symptoms and your health.
Weight loss surgery may be considered in women who have a BMI over 40.
There is no strong evidence that PCOS by itself can cause you to gain weight or makes losing weight difficult. Many women find great benefit from support groups such as Verity
Have regular health checks
Once you have a diagnosis of PCOS, you should be monitored to check for any early signs of health problems:
- Diabetes: Depending on your risk factors, you may be offered testing for diabetes every 1 - 3 years.
- Cancer of the womb: It is important to have a period every 3-4 months to reduce the risk of excessive thickening of the lining of the uterus. If you have not had a period for over 4 months, you may need hormone tablets to make you have a period. You may also be offered further tests such as an ultrasound scan of your uterus.
- High blood pressure: Discuss with your doctor how often you should have your blood pressure checked and whether you should have blood tests to check your cholesterol levels.
- Depression and psychological problems: You can be referred to a counsellor or trained specialist if necessary.
There is no cure for PCOS. Medical treatments aim to manage and reduce the symptoms or consequences of having PCOS. Medication alone has not been shown to be any better than healthy lifestyle changes (weight loss and exercise).
Many women with PCOS successfully manage their symptoms and long-term health risks without medical intervention. They do this by eating a healthy diet, exercising regularly and maintaining a healthy lifestyle.
If you are asked to make a choice, you may have lots of questions that you want to ask. You may also want to talk over your options with your family or friends. It can help to write a list of the questions you want answered and take it to your appointment.
Ask 3 Questions
To begin with, try to make sure you get the answers to 3 key questions, if you are asked to make a choice about your healthcare:
- What are my options?
- What are the pros and cons of each option for me?
- How do I get support to help me make a decision that is right for me?
*Ask 3 Questions is based on Shepherd et al. Three questions that patients can ask to improve the quality of information physicians give about treatment options: A cross-over trial. Patient Education and Counselling, 2011;84:379-85
Sources and acknowledgements
This information has been developed by the RCOG Patient Information Committee. It is based on the RCOG Green-top Clinical Guideline Long-term Consequences of Polycystic Ovary Syndrome (November 2014). The guideline contains a full list of the sources of evidence we have used.
This information was reviewed before publication by women attending clinics in Leeds, Cheshire and London, by the RCOG Women’s Network and by the RCOG Women’s Voices Involvement Panel.
