Published: June 2023
Please note that this information will be reviewed every 3 years after publication.
This information is for you if you have had three or more early (in the first three months of pregnancy) miscarriages.
It may also be helpful if you are a partner, relative or friend of someone in this difficult situation.
It tells you about:
- Possible reasons for your miscarriages
- Investigations that you may be offered
- Possible options for treatment.
This information does not cover the treatment of a miscarriage at the time that it happens. Please see the RCOG patient information Early Miscarriage for information about the immediate diagnosis and treatment of miscarriage.
The information here aims to help you better understand your health and your options for treatment and care. Your healthcare team is there to support you in making decisions that are right for you. They can help by discussing your situation with you and answering your questions.
Within this information we may use the terms ‘woman’ and ‘women’. However, we know that it is not only people who identify as women who may want to access this leaflet. Your care should be appropriate, inclusive and sensitive to your needs whatever your gender identity.
Miscarriages are often emotionally very difficult. Recurrent miscarriage can cause considerable distress, and concern about your future. You can find further information and support from your healthcare professional and the organisations listed at the end of this leaflet.
A glossary of medical terms is available at A-Z of medical terms.
Key points
- Recurrent miscarriage is when you have had three or more early miscarriages.
- Most cases of recurrent miscarriage are unexplained. However, there are many different things which may make a miscarriage more likely. These include being older, being very underor overweight, smoking, and drinking excessive alcohol or caffeine. There can be problems with the way your blood clots, the shape of your womb, your hormones or genetics.
- You will be offered investigations to see if there is a reason for recurrent miscarriage. If a possible reason is found, there may be treatment available to improve your chances of a successful pregnancy.
- If recurrent miscarriage is unexplained, most women will have a good chance of a successful pregnancy in the future, with support from their healthcare team.
If you lose a pregnancy or baby before 24 weeks of pregnancy, it is called a miscarriage. If this happens in the first 3months of pregnancy, it is known as a first trimester or early miscarriage. Other forms of pregnancy loss (ectopic pregnancy or molar pregnancy) can happen before 24 weeks but they are not covered in this leaflet. For further information, please see RCOG patient information Ectopic pregnancy and RCOG patient information Molar pregnancy.
When an early miscarriage happens three or more times, it is called recurrent miscarriage. These miscarriages do not have to happen one after the next, and you may have healthy pregnancies in between. Recurrent miscarriage affects 1 in 100 (1%) women.
There are a number of factors that make miscarriage more likely:
Genetic factors
The most common cause of one miscarriage, or of recurrent miscarriage, is that the pregnancy has developed with abnormal chromosomes. 1 in 2 (50%) miscarriages happen because of this, and it gets more common as parents get older.
In most cases, this happens even though the parents themselves have normal chromosomes. However, in 6 in 100 (6%) couples who have experienced three miscarriages, one parent may have their own chromosomes in an abnormal arrangement. Although this does not affect the parent, if it is passed on to the embryo it can cause a miscarriage.
Age
The older you are, the more likely you are to have a single miscarriage, or to have recurrent miscarriage. This is because as you get older the quality of your eggs declines.
Age-related risk of miscarriage:
| Age of mother | Risk of miscarriage |
| Under 35 years | 11 to 15 in 100 women (11 to 15%) |
| 35 - 39 years | 25 in 100 women (25%) |
| 40 - 44 years | 51 in 100 women (51%) |
| Over 45 years |
93 in 100 women (93%) |
Miscarriages may also be more common if the father is more than 40 years old.
Ethnicity
If you are of Black African or Black Caribbean background, you are more likely to have an early miscarriage. We do not fully understand at present why this is.
Lifestyle factors
Being overweight (body mass index (BMI) more than 25) or underweight (BMI less than 19) increases your chance of having one or more miscarriages. Cigarette smoking and drinking more than the recommended amount of alcohol or caffeine may also increase your chance of miscarriage.
Blood clotting factors
Antiphospholipid syndrome (APS): this is a condition that can cause you to have recurrent miscarriage or later pregnancy complications. It also puts you at risk of developing blood clots.
Inherited blood clotting problems (thrombophilia): there are several different types of inherited blood clotting problems. Testing for them is not recommended, as there is no clear evidence that these can cause you to have recurrent miscarriage.
Abnormalities in the shape of your uterus (womb)
Five to six in 100 women are born with a uterus that is an unusual shape, known as a ‘congenital uterine anomaly’. In women with recurrent miscarriage, it is more common to have a uterus that is an unusual shape (around 13 in 100 women).
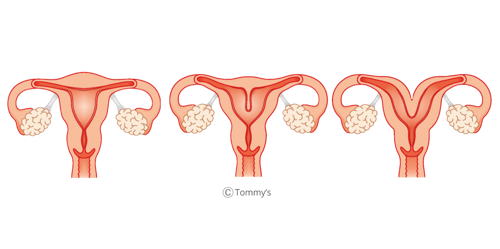
Certain uterine shapes may increase your chance of miscarriage, such as a septate uterus and a bicornuate uterus. A septate uterus is when there is a thin wall of tissue in the middle of the uterus. A bicornuate uterus is where there is a deep indentation of the muscle at the top of the uterus, dividing it into two halves.
Normal : Septate Uterus : Bicornuate uterus
Some women develop fibroids (knots of muscle in the wall of the uterus), or scar tissue within their uterus, over their lifetime. How they affect you, and whether they affect your chance of miscarriage, may depend on their size and position. You may wish to discuss this further with your healthcare professional. We do not yet fully understand when treatment might improve your chances of a healthy pregnancy.
Hormonal problems
There are several different hormonal conditions that may be related to miscarriage:
- Diabetes: Well-controlled diabetes does not increase your risk of miscarriage. However, if you have poorly controlled diabetes you may have a higher chance of miscarriage.
- Thyroid problems – Well-controlled thyroid disease does not cause miscarriage. However, high levels of the ‘thyroid stimulating hormone’ (TSH) or the presence of thyroid antibodies, may put you at higher risk of miscarriage.
- Polycystic ovarian syndrome (PCOS) - Women with PCOS are at increased risk of miscarriage. It is not clear why this is, but it could be due to the raised insulin and testosterone hormones that are sometimes seen in this condition.
- Prolactin imbalances - If you have abnormal prolactin hormone levels you may be at increased risk of miscarriage.
Immune factors
It has been suggested that some women miscarry because their immune system does not respond normally to pregnancy. There is no clear evidence to support this theory at present and further research is needed.
Sperm factors
If your partner has abnormal DNA in their sperm, there may be a higher possibility of recurrent miscarriage. We do not currently have any good evidence that we can change sperm health to reduce the risk of miscarriage, and therefore testing of sperm is not usually offered.
Finding out whether or not there is a reason or treatable cause for your recurrent miscarriages is important so that you can be offered the support and treatment that is best for you. You should see your healthcare professional for referral for further investigations, which may be arranged in a clinic dedicated to recurrent miscarriage. If possible, you and your partner should be seen together.
Sometimes it can take time to arrange, or time to get the results from, these investigations. It is up to you whether you continue to try for a pregnancy while you wait for the results of these investigations, and you may wish to discuss this with your healthcare professional.
Blood tests
- APS test: To confirm if you have APS you need to have positive results on two blood tests at least 12 weeks apart, and at least 6 weeks after a miscarriage.
- Thyroid tests including thyroid antibody tests.
- Diabetes tests if your medical history suggests this could be a factor.
If your healthcare professional suspects that you may have other hormonal problems, such as PCOS or prolactin imbalance, you will be offered blood tests to check for these.
Genetic tests
At the time of your third or further miscarriage, your healthcare professional should offer to test whether there were any inherited chromosomal problems causing this miscarriage.
Both you and your partner may be offered genetic testing if:
- it has not been possible to test the pregnancy, or
- the testing of the pregnancy suggests the problem could have been inherited.
A scan of your uterus
You should be offered a pelvic ultrasound scan to look at the shape of your uterus. If your healthcare professional suspects that your uterus is an unusual shape, you may be offered further investigations to look at this in more detail.
Lifestyle modifications
Your healthcare professional will discuss with you how to maintain a healthy weight. They can support you in stopping smoking. You should limit the amount of caffeine you drink to less than 200 mg/day (around two cups of tea or instant coffee), and should avoid drinking alcohol regularly or to excess.
Treatment for Antiphospholipid syndrome (APS)
If you have APS and have had recurrent miscarriages, treatment with low-dose aspirin tablets and blood thinning injections (heparin) in pregnancy can increase your chance of having a successful pregnancy. Aspirin and heparin make your blood less likely to clot.
Having APS means you are at increased risk of complications throughout your pregnancy so you will be closely monitored by your healthcare team.
Treatment for inherited thrombophilia
Routine treatment for inherited thrombophilia has not been found to improve your chance of a healthy pregnancy. If you have been found to have an inherited blood clotting condition, you may be offered heparin. If you are known to have an inherited blood clotting condition, you may be offered treatment by your healthcare professional. This will depend on your individual circumstances and your additional risks of developing blood clots during pregnancy.
Referral for genetic counselling
If either you or your partner is found to have a genetic abnormality, you should be offered the chance to see a genetics counsellor. They will discuss your chances of future miscarriage and will explain what your options are depending on your individual circumstances.
Surgery to your uterus
If you have a uterine septum you may be offered an operation to correct this. It is unclear whether surgery for fibroids or other conditions affecting the internal shape of your womb reduces your risk of miscarriage. The potential benefits and risks of having surgery on your uterus should be discussed with you by your healthcare professional, depending on your individual circumstances (for example, the size and position of a fibroid).
Hormone treatment
If you have diabetes or thyroid disease, you will be supported to control this as well as possible before your next pregnancy.
There is no evidence that progesterone treatment prevents recurrent miscarriage unless you experience bleeding in early pregnancy. If you have had a previous miscarriage and are bleeding in pregnancy, you should be offered progesterone to try to prevent miscarriage.
It is very common that recurrent miscarriage is unexplained. In this situation, there is currently no evidence that any form of medical treatment will reduce your chance of a further miscarriage. Your chance of a successful pregnancy next time will depend on your individual circumstances but is likely to be good, even without changing anything.
It may be important in your future pregnancies to have supportive care from healthcare professionals who are experienced in caring for women with recurrent miscarriage. This may include having ultrasound scans for reassurance.
Your chance of another miscarriage depends on many factors, including the number of miscarriages you have experienced, your age, and the results of your investigations.
Tommy’s charity has developed a tool, which allows you to estimate the chances of your next pregnancy being successful. If you think you would find this helpful, you can access this tool via the Tommy's website.
Having recurrent miscarriage can be a difficult experience which may affect you physically and emotionally. You and your partner should be offered information and support by your healthcare professionals and support groups are available.
Some people experience significant symptoms of anxiety, depression and/or post-traumatic stress after pregnancy loss. You may wish to discuss your mental health with your healthcare professional, as you can be offered referral for further support and treatment.
Further support
Phone line: +44 (0)1924 200799
Further information
If you are asked to make a choice, you may have lots of questions that you want to ask. You may also want to talk over your options with your family or friends. It can help to write a list of the questions you want answered and take it to your appointment.
Ask 3 Questions
To begin with, try to make sure you get the answers to 3 key questions, if you are asked to make a choice about your healthcare:
- What are my options?
- What are the pros and cons of each option for me?
- How do I get support to help me make a decision that is right for me?
*Ask 3 Questions is based on Shepherd et al. Three questions that patients can ask to improve the quality of information physicians give about treatment options: A cross-over trial. Patient Education and Counselling, 2011;84:379-85
Sources and acknowledgements
This information has been developed by the RCOG Patient Information Committee. The image for uterus shapes was provided by Tommy’s. This information is based on the RCOG Green-top Guideline No 17 on Recurrent miscarriage published in June 2023. The guideline contains a full list of the sources of evidence we have used.
