Published: June 2019
Please note that this information will be reviewed every 3 years after publication.
To access this leaflet in additional languages, please visit our Translations page.
This information is for you if you think that, or have been told that, your waters have broken early but you have not gone into labour.
It may also be helpful if you are a partner, friend or relative of someone who is in this situation.
This applies to you if your waters may have broken between 24 and 37 completed weeks of pregnancy.
If your waters break before 24 weeks, you should have a discussion with your healthcare professional about your individual circumstances.
The information here aims to help you better understand your health and your options for treatment and care. Your healthcare team is there to support you in making decisions that are right for you. They can help by discussing your situation with you and answering your questions.
This information covers:
- What Preterm Prelabour Rupture of Membranes (PPROM) is
- What you should do if you have PPROM
- What happens at hospital and if PPROM is diagnosed
- What PPROM could mean for you and your baby
- Treatment options
- Information about giving birth
- What PPROM means for future pregnancies
- Further information and support available
Within this information, we may use the terms ‘woman’ and ‘women’. However, it is not only people who identify as women who may want to access this information. Your care should be personalised, inclusive and sensitive to your needs, whatever your gender identity.
A glossary of medical terms is available at A-Z of medical terms.
Key points
- Preterm prelabour rupture of membranes (PPROM) is when your waters break before 37 completed weeks of pregnancy but you haven’t gone into labour yet.
- If this happens, you have a higher chance of giving birth prematurely and there is an increased chance that both you and your baby may develop an infection that can make you both unwell.
- You will be offered a course of antibiotics to reduce the risk of an infection developing and to help the pregnancy to continue.
- If you are well with no signs of infection and your baby is growing well in your uterus (womb), then it may be better to allow your pregnancy to continue until 37 weeks. You will be monitored very closely for any signs of infection by your healthcare team, and your individual circumstances and preferences will be taken into account.
- If you or your baby show any signs of infection or develop other complications, you may need to give birth to your baby straight away.
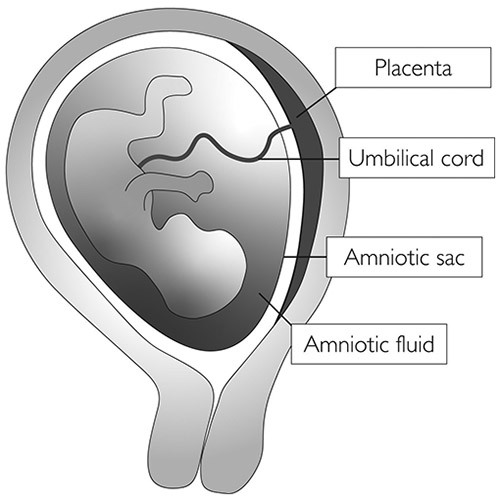
Your baby is surrounded by amniotic fluid or ‘waters’ contained within a membrane bag (the amniotic sac) inside your uterus.
When the waters break, it is also known as rupture of the membranes.
Normally your waters break shortly before or during labour.
If your waters break before labour at less than 37 weeks of pregnancy, this is known as preterm prelabour rupture of membranes (PPROM).
This can happen in up to 3 out of every 100 (3%) pregnant women.
PPROM is associated with 3-4 out of every 10 preterm births.
The reason why PPROM happens is not always known, but may be because of infections, placental problems or other causes.
Diagram showing a baby in the womb, marking the placenta, umbilical cord, amniotic sac and amniotic fluid:
You may notice a ‘gush’ of fluid or you may feel damp. The amount of fluid you lose may vary from a trickle to a gush.
If you think that you are leaking fluid from the vagina, wear a pad not a tampon and note the colour and amount of the fluid.
Leaking urine is common while you’re pregnant, but if you think your waters may have broken, you should contact your healthcare professional and go to the hospital for a check-up straight away.
You will have a check-up that should include:
- a discussion with your healthcare professional about what has happened, including details about the fluid loss, how you are feeling, how your pregnancy has been so far and whether you have any risk factors for PPROM or preterm birth (for example, if this has happened in previous pregnancies it is more likely to happen again)
- a check of your general health, including an examination and a check of your temperature, pulse and blood pressure
- a check of your baby’s heartbeat.
- PPROM is best diagnosed by a vaginal examination. With your consent, your healthcare professional will use a sterile speculum (an instrument used to separate the walls of the vagina) to look at your cervix and see whether the leaking fluid is amniotic fluid.
- A swab test of the fluid may help to decide whether your waters have broken, if it is still unclear after the speculum examination.
- An ultrasound scan to estimate the amount of fluid around your baby is sometimes helpful.
If your waters have broken, you will usually be advised to stay in hospital for a few days, although in some situations this may be for longer.
You and your baby will be closely monitored for signs of infection.
This will include having your temperature, blood pressure and pulse taken regularly, together with blood tests to check for infection.
Your baby’s heart rate will also be monitored regularly.
If your waters have not broken, you should be able to go home.
If only a very small amount of amniotic fluid is leaking, it is not always easy to see on examination and it can be difficult to confirm whether your waters have broken.
If you continue to leak fluid at home, you should return to the hospital for a further check-up.
Infection
The membranes form a protective barrier around the baby, and after these have broken, there is a risk of infection getting into your uterus (chorioamnionitis). If you have an infection, this can cause you to go into labour early or cause you or your baby to develop sepsis.
The symptoms of infection include a raised temperature, an unusual vaginal discharge with an unpleasant smell, a fast pulse rate and pain in your lower abdomen. Your baby’s heart rate may also be faster than normal.
If there are signs that you have an infection, your baby may need to be born straight away to try to prevent both you and your baby becoming more unwell.
Preterm birth
About 50% of women with PPROM will go into labour within the first week after their waters break. The further along you are in your pregnancy the more likely you are to go into labour within 1 week of your waters breaking.
Problems of prematurity
Babies born prematurely have an increased risk of health problems, particularly with breathing, feeding and infection, and may need admission to a neonatal unit. The earlier your baby is born, the more likely that this will be the case.
If your waters have broken early, your healthcare professional will discuss with you the possible outcomes for your baby, depending on how many weeks pregnant you are when this happens and on your individual circumstances.
Other complications
- Cord prolapse, when the umbilical cord falls through your cervix into the vagina: this is an emergency complication and can be life-threatening for your baby, but it is uncommon.
- Pulmonary hypoplasia, when your baby’s lungs fail to develop normally because of a lack of fluid around them: this is more common if your waters break very early on in pregnancy (less than 24 weeks) when your baby’s lungs are still developing.
- Placental abruption, when your placenta separates prematurely from your uterus: this can cause heavy bleeding and can be dangerous for both you and your baby.
If you experience PPROM, sometimes your baby may not survive. The risk of this happening is greater if your waters break very early, if the baby is born very prematurely or, in some cases, following infection or cord prolapse.
It is not possible to replace the fluid or repair the hole in the membranes around your baby. You may carry on leaking fluid for the rest of your pregnancy as amniotic fluid continues to be made.
However, treatment may be offered to reduce the risk to your baby. This could include:
- a course of antibiotic tablets to reduce the risk of an infection getting into the uterus and affecting both you and your baby; antibiotics can also help to delay you going into labour
- a course of steroid injections (corticosteroids) to help with your baby’s development and to reduce the chance of problems caused by being born preterm; see the RCOG patient information Corticosteroids in pregnancy to reduce complications from being born prematurely
- magnesium sulfate, a medication that may be offered to you if your baby is at risk of being born very prematurely; this can reduce the risk of them developing cerebral palsy
- intravenous antibiotics (if you are in preterm labour) to reduce the risk of early-onset group B Streptococcus (GBS) infection; see the RCOG patient information Group B Streptococcus (GBS) in pregnancy and newborn babies.
You will usually be advised to stay in hospital for a few days after your waters break, to monitor both your and your baby’s wellbeing. Your healthcare professional will discuss with you the option of going home after this time, if you are well and not considered to be at higher risk for giving birth early.
Before going home from hospital, your healthcare professional will give you information on symptoms to look out for. Contact your healthcare professional and return to the hospital immediately if you experience any of the following:
- raised temperature
- flu-like symptoms (feeling hot and shivery)
- vaginal bleeding
- if the leaking fluid becomes greenish or smelly
- contractions or cramping pain
- abdominal pain or back pain
- if you are worried that the baby is not moving as normal.
You should have regular check-ups with your healthcare professional (usually one or two times per week).
During these check-ups, your baby’s heart rate will be monitored, your temperature, pulse and blood pressure will be checked and you will have blood tests looking for signs of infection.
Your obstetrician will work with you to make an ongoing plan for your pregnancy.
Experiencing PPROM can be a very stressful time for both you and your family.
You should be offered emotional support during your pregnancy and after your baby is born.
If you are worried about how you are feeling, do seek help from your healthcare professional and support groups (see links below).
If you and your baby are both well with no signs of infection then you may be advised to wait until 37 weeks to give birth. This is because carrying on with the pregnancy reduces the risk to your baby that are related to being born preterm.
If you are known to carry the GBS bacteria, then you may be advised to give birth from 34 weeks because of the risk of GBS infection in your baby. See the RCOG patient information Group B Streptococcus (GBS) in pregnancy and newborn babies.
Your healthcare professional should discuss the timing of birth with you depending on your individual circumstances and preferences. You will have the opportunity to ask any questions you have about your pregnancy and about preparing for birth.
It is often possible to have a vaginal birth after PPROM but this will depend on when you go into labour, the position your baby is lying in in your uterus, and your own individual circumstances and choices.
Your healthcare professional will discuss this with you.
Having PPROM or giving birth prematurely means that you are at an increased risk of having a preterm birth in any future pregnancies.
You will be advised to be under the care of a specialist team who will discuss with you a plan for your pregnancy depending on your individual situation.
The nature of gynaecological and obstetric care means that intimate examinations are often necessary.
We understand that for some people, particularly those who may have anxiety or who have experienced trauma, physical abuse or sexual abuse, such examinations can be very difficult.
If you feel uncomfortable, anxious or distressed at any time before, during or after an examination, please let your healthcare professional know.
If you find this difficult to talk about, you may communicate your feelings in writing.
Your healthcare professionals are there to help and they can offer alternative options and support for you.
Remember that you can always ask them to stop at any time and that you are entitled to ask for a chaperone to be present. You can also bring a friend or relative if you wish.
Further information
NICE guideline NG25, Preterm Labour and Birth
RCOG Green-top Guideline No. 73, Care of Women Presenting with Suspected Preterm Prelabour Rupture of Membranes from 24+0 Weeks of Gestation
RCOG patient information: Umbilical cord prolapse in late pregnancy
Sources and acknowledgements
This information has been developed by the RCOG Patient Information Committee. It is based on the RCOG Green-top Guideline No. 73, Care of Women Presenting with Suspected Preterm Prelabour Rupture of Membranes from 24+0 Weeks of Gestation, published in June 2019. The guideline contains a full list of the sources of evidence we have used.
This information has been reviewed before publication by members of the RCOG Women’s Network and the RCOG Women’s Voices Involvement Panel and by women attending clinics across the UK.
