This information is for you if you want to know more about ectopic pregnancy, how it is diagnosed and how it is treated.
It may also be helpful if you are a relative, partner or friend of someone with a suspected or confirmed ectopic pregnancy.
The information here aims to help you better understand your health and your options for treatment and care. Your healthcare team is there to support you in making decisions that are right for you. They can help by discussing your situation with you and answering your questions.
Information covered in this leaflet:
- What an ectopic pregnancy is
- What a pregnancy of unknown location or PUL is
- What the symptoms of an ectopic pregnancy are
- When you should seek medical advice if you think you may have an ectopic pregnancy
- Who is at increased risk of ectopic pregnancy
- How an ectopic pregnancy is diagnosed
- What happens when an ectopic pregnancy is suspected or diagnosed
- The options available for treatment of ectopic pregnancy
- Future pregnancies after an ectopic pregnancy
- Further information and support available
This leaflet is mainly about an ectopic pregnancy in the fallopian tube (tubal ectopic pregnancy), although it does provide some information on ectopic pregnancy at sites other than the fallopian tubes (non-tubal ectopic pregnancy).
Within this information, we may use the terms ‘woman’ and ‘women’. However, it is not only people who identify as women who may want to access this information. Your care should be personalised, inclusive and sensitive to your needs, whatever your gender identity.
A glossary of medical terms is available at A-Z of medical terms.
Key points
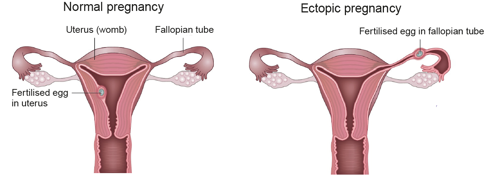
- An ectopic pregnancy is a pregnancy outside the uterus (womb).
- In the UK, 1 in 90 pregnancies (just over 1%) is an ectopic pregnancy.
- Most ectopic pregnancies develop in the fallopian tubes (tubal pregnancy) but in rare cases they can develop at other sites.
- Diagnosis is made based on your symptoms, examination(s), blood tests, scan and other tests as appropriate.
- Treatment options vary depending on the location of your ectopic pregnancy and the results of your tests.
An ectopic pregnancy is one that grows outside the uterus (womb). In the UK, 1 in 90 pregnancies (just over 1%) is an ectopic pregnancy. Women who have had a previous ectopic pregnancy are at higher risk. A pregnancy cannot survive in these situations and it can pose a serious risk to you.
In a normal pregnancy, the fertilised egg moves from the fallopian tube into the uterus, where the pregnancy grows and develops. If this does not happen, the fertilised egg may implant and start to develop outside the uterus, leading to an ectopic pregnancy.
An ectopic pregnancy can be life-threatening because as the pregnancy gets bigger it can burst (rupture), causing severe pain and internal bleeding.
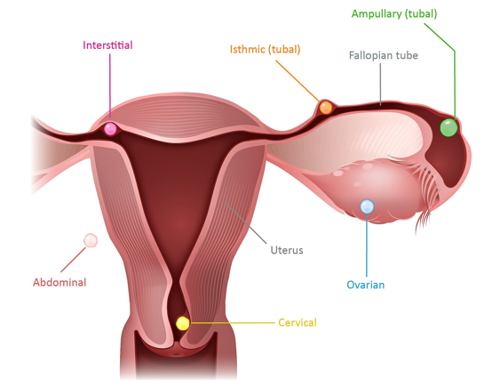
Most ectopic pregnancies develop in the fallopian tubes (tubal pregnancy) but, rarely (3–5 out of 100 ectopic pregnancies), they can occur in other places.
The image below shows some of these sites.
A pregnancy of unknown location (PUL) means that you have a positive pregnancy test but there is no identified pregnancy on an ultrasound scan.
This may be due to three possible reasons:
- you may have a very early pregnancy within the uterus that is too small to be seen on a scan
- you may have miscarried; your pregnancy test can remain positive for up to 2–3 weeks following a miscarriage
- you may have an ectopic pregnancy.
Uncertainty about your pregnancy can be very stressful for you and your family. While it may take time, it is important to reach the correct diagnosis before your doctor discusses your treatment options with you. With a PUL, you will be advised to have regular blood tests to measure your pregnancy hormone levels and your treatment plan will be based on the results of these blood tests, ultrasound scan reports and clinical features.
Each woman is affected differently by an ectopic pregnancy. Some women have no symptoms, some have a few symptoms, while others have many symptoms. Most women get physical symptoms in the 6th week of pregnancy (about 2 weeks after a missed period). You may or may not be aware that you are pregnant if your periods are irregular, or if the contraception you are using has failed.
Because symptoms vary so much, it is not always straightforward to reach a diagnosis of an ectopic pregnancy.
The symptoms of an ectopic pregnancy may include:
- pain in your lower abdomen. This may develop suddenly for no apparent reason or may come on gradually over several days. It may be on one side only.
- vaginal bleeding. You may have some spotting or bleeding that is different from your normal period. The bleeding may be lighter or heavier or darker than normal.
- pain in the tip of your shoulder. This pain is caused by blood leaking into the abdomen and is a sign that the condition is getting worse. This pain is there all the time and may be worse when you are lying down. It is not helped by movement and may not be relieved by painkillers. You should seek urgent medical advice if you experience this.
- upset tummy. You may have diarrhoea, or feel pain on opening your bowels.
- severe abdominal pain/collapse. If the fallopian tube bursts (ruptures) and causes internal bleeding, you may develop intense abdominal pain or you may collapse. In rare instances, collapse may be the very first sign of an ectopic pregnancy. This is an emergency situation and you should seek urgent medical attention.
Yes. An ectopic pregnancy can pose a serious risk to your health. If you have had sex within the last 3 or 4 months (even if you have used contraception) and are experiencing these symptoms, you should get medical help immediately. Seek advice even if you do not think you could be pregnant.
You can get medical advice from:
- your GP or midwife
- the A&E department at your local hospital
- an Early Pregnancy Assessment Unit (EPAU); details of the unit nearest to you can be found at: www.aepu.org.uk/find-a-unit
- NHS 111 (England and Wales) and NHS 24 (Scotland) on 111; support is available 24 hours a day, 365 days a year, by dialing 111; calls are free from landlines and mobile phones.
Any sexually active woman of childbearing age could have an ectopic pregnancy. You have an increased risk of an ectopic pregnancy if:
- you have had a previous ectopic pregnancy
- you have a damaged fallopian tube; the main causes of damage are:
- previous surgery to your fallopian tubes, including sterilisation
- previous infection in your fallopian tubes; see the RCOG patient information Acute pelvic inflammatory disease
- you become pregnant when you have an intrauterine device (IUD/coil) or if you are on the progesterone-only contraceptive pill (mini pill)
- your pregnancy is a result of assisted conception, i.e. in vitro fertilisation (IVF) or intracytoplasmic sperm injection (ICSI)
- you smoke.
Most ectopic pregnancies are suspected between 6 and 10 weeks of pregnancy. Sometimes the diagnosis is made quickly. However, if you are in the early stages of pregnancy, it can take longer (a week or more) to make a diagnosis of an ectopic pregnancy.
Your diagnosis will be made based on the following:
- Consultation and examination. Your doctor will ask about your medical history and symptoms, and will examine your abdomen. With your consent, your doctor may also do a vaginal (internal) examination. You should be offered a female chaperone (someone to accompany you) for this. You may also wish to bring someone to support you during your examination.
- Urine pregnancy test. If you have not already had a positive pregnancy test, you will be asked for a urine sample so that this can be tested for pregnancy. If the pregnancy test is negative, it is very unlikely that your symptoms are due to an ectopic pregnancy.
- Ultrasound scan. A transvaginal scan (where a probe is gently inserted in your vagina) is known to be more accurate in diagnosing an ectopic pregnancy than a scan through the tummy (transabdominal scan). Therefore, you will be offered a transvaginal scan to help identify the exact location of your pregnancy. However, if you are in the early stages of pregnancy, it may be difficult to locate the pregnancy on scanning and you may be offered another scan after a few days.
- Blood tests. A test for the level of the pregnancy hormone βhCG (beta human chorionic gonadotrophin) or a test every few days to look for changes in the level of this hormone may help to give a diagnosis. This is usually checked every 48 hours because, with a pregnancy in the uterus, the hormone level rises by 63% every 48 hours (known as the ‘doubling time’) whereas, with ectopic pregnancies, the levels are usually lower and rise more slowly or stay the same.
- Laparoscopy. If the diagnosis is still unclear, an operation under a general anaesthetic called a laparoscopy may be necessary. The doctor uses a small telescope to look at your pelvis by making a tiny cut, usually into the umbilicus (tummy button). This is also called keyhole surgery. See the RCOG patient information Recovering well: information for you after a laparoscopy. If an ectopic pregnancy is confirmed, treatment may be undertaken as part of the same operation. This would be discussed with you before surgery, unless surgery is necessary due to an acute emergency situation.
When an ectopic pregnancy is suspected or confirmed, your doctor will discuss your treatment options with you. The options usually depend on where the ectopic pregnancy is suspected or located.
Make sure that you:
- fully understand all your options
- ask for more information if there is something you do not understand
- raise your concerns, if any
- understand what each option means for your fertility (see the section below on What about future pregnancies?)
- have enough time to make your decision.
Because an ectopic pregnancy cannot lead to the birth of a baby, all options will end the pregnancy in order to reduce the risks to your own health.
Your options depend upon:
- how many weeks pregnant you are
- your symptoms and clinical condition
- the level of βhCG
- your scan result
- your fertility status
- your general health
- your personal views and preferences – this should involve a discussion about your future pregnancy plans
- the options available at your local hospital.
The treatment options for tubal ectopic pregnancy are listed below – not all may be suitable for you, so your healthcare professional should guide you in making an informed decision.
Expectant management (wait and see)
Ectopic pregnancies sometimes end on their own – similar to a miscarriage. Depending on your situation, it may be possible to monitor the βhCG levels with blood tests every few days until these are back to normal. Although you do not have to stay in hospital, you should go back to hospital if you have any further symptoms (see the section above on What are the symptoms of an ectopic pregnancy?). You should be given a direct contact number for the emergency ward or gynaecology ward at your hospital.
Expectant management is not an option for all women. It is usually only possible when the pregnancy is still in the early stages and when you have only a few or no symptoms. Success rates with expectant management are highly variable and range from 30% to 100%. This mainly depends on your pregnancy hormone levels, with higher serum βhCG levels associated with a lower chance of success.
Medical treatment
In certain circumstances, an ectopic pregnancy may be treated by medication (drugs). The fallopian tube is not removed. A drug (methotrexate) is given as an injection – this prevents the ectopic pregnancy from growing and the ectopic pregnancy gradually disappears.
Most women only need one injection of methotrexate for treatment. However, 15 in 100 women (15%) need to have a second injection of methotrexate. If your pregnancy is beyond the very early stages or the βhCG level is high, methotrexate is less likely to succeed. Seven in 100 women (7%) will need surgery even after medical treatment.
Many women experience some pain in the first few days after taking the methotrexate, but this usually settles with paracetamol or similar pain relief. Although it is known that long-term treatment with methotrexate for other illnesses can cause significant side effects, this is rarely the case with one or two injections as used to treat ectopic pregnancy. Treatment of ectopic pregnancy with methotrexate is not known to affect the capacity of your ovaries to produce eggs.
You may need to stay in hospital overnight and then return to the clinic or ward a few days later. You will be asked to return sooner if you have any symptoms. It is very important that you attend your follow-up appointments until your pregnancy hormone levels are back to normal. You are also advised to wait for 3 months after the injection before you try for another pregnancy.
Surgical treatment
An operation to remove the ectopic pregnancy will involve a general anaesthetic.
The surgery will either be:
- Laparoscopy (known as keyhole surgery). Your stay in hospital is shorter (24–36 hours) and physical recovery is quicker than after open surgery. See the RCOG patient information Recovering well: information for you after a laparoscopy. Laparoscopy might not be an option for some women and your doctor will discuss this with you.
- Open surgery (known as a laparotomy). This is done through a larger cut in your abdomen and may be needed if severe internal bleeding is suspected. You will need to stay in hospital for 2–4 days. It usually takes about 4–6 weeks to recover.
The aim of surgery is to remove the ectopic pregnancy. The type of operation you have will depend on your wishes or plans for a future pregnancy and what your surgeon finds during the operation (laparoscopy).
To have the best chance of a future pregnancy inside your uterus, and to reduce the risk of having another ectopic pregnancy, you will usually be advised to have your affected fallopian tube removed (this is known as a salpingectomy).
If you already have only one fallopian tube or your other tube does not look healthy, your chances of getting pregnant are already affected. In this circumstance, you may be advised to have a different operation (known as a salpingotomy) that aims to remove the pregnancy without removing the tube. It carries a higher risk of a future ectopic pregnancy but means that you are still able to have a pregnancy in the uterus in the future. You will be advised to have blood tests for checking your pregnancy hormone levels after salpingotomy as part of follow-up. Some women may need further medical treatment or another operation to remove the tube later if the pregnancy has not been completely removed during salpingotomy. The decision to perform salpingectomy or salpingotomy may sometimes only be made during laparoscopy under anaesthetic. There are risks associated with any operation: from the surgery itself and from the use of an anaesthetic. Your surgeon and anaesthetist will discuss these risks with you.
The treatment of a non-tubal ectopic pregnancy depends on where the pregnancy is growing (refer to the various sites of non-tubal ectopic pregnancy in the leaflet). Your doctor will discuss the available treatment options with you based on a number of factors, including the location of the ectopic pregnancy, the levels of the pregnancy hormone βhCG in your blood and the ultrasound scan report.
Treatment options may include expectant management, medical treatment with methotrexate or surgical operation.
If the tubal or non-tubal pregnancy has burst, emergency surgery is needed to stop the bleeding. This operation is often life-saving. It is done by removing the ruptured fallopian tube and pregnancy. Your doctors will need to act quickly and this may mean that they have to make a decision on your behalf to operate. In this situation you may need a blood transfusion. See the RCOG patient information Blood transfusion, pregnancy and birth.
To confirm that you have had an ectopic pregnancy, tissue removed at the time of surgery is sent for testing in the laboratory. The healthcare team will discuss with you (and your partner) the options around what happens to your pregnancy remains afterwards.
Follow-up appointments
It is important that you attend your follow-up appointments. The check-ups and tests that you need will depend on the treatment that you had. If you had treatment with methotrexate, you should avoid getting pregnant for at least 3 months after the injection.
How will I feel afterwards?
The impact of an ectopic pregnancy can be very significant. It might mean coming to terms with the loss of your baby, with the potential impact on future fertility, or with the realisation that you could have lost your life.
Each woman copes in her own way. An ectopic pregnancy is a very personal experience. This experience may affect your partner and others in your family, as well as close friends.
If you feel you are not coping or not getting back to normal, you should talk to your GP or another member of your healthcare team. See also the Further information section below for details of organisations that can provide advice and support.
It is important to remember that the pregnancy could not have continued without causing a serious risk to your health.
Before trying for another baby, it is important to wait until you feel ready emotionally and physically. However traumatic your experience of an ectopic pregnancy has been, it may help to know that the likelihood of a normal pregnancy next time is much greater than that of having another ectopic pregnancy.
What about future pregnancies?
The chances of having a successful pregnancy in the future are good. Even if you have only one fallopian tube, your chances of conceiving are only slightly reduced.
For most women an ectopic pregnancy is a ‘one-off’ event. However, your overall chance of having another ectopic pregnancy is increased and is around 7–10 in 100 (7–10%) compared with 1 in 90 (just over 1%) in the general UK population.
You should seek early advice from a healthcare professional when you know you are pregnant. You may be offered an ultrasound scan at between 6 and 8 weeks to confirm that the pregnancy is developing in the uterus.
If you do not want to become pregnant, seek further advice from your doctor or family planning clinic, as some forms of contraception may be more suitable after an ectopic pregnancy.
Further information
Tommy’s information on cctopic pregnancy
Association of Early Pregnancy Units
NICE patient information on ectopic pregnancy and miscarriage
Sources and acknowledgements
This information has been developed by the RCOG Patient Information Committee. It is based on the RCOG Green-top Guideline Diagnosis and Management of Ectopic Pregnancy, which contains a full list of the sources of evidence we have used.
This information was reviewed before publication by women attending clinics at hospitals in Chesterfield, Nottingham, Essex, Inverness, Liverpool, Manchester, London, Bristol, Sussex and Basildon, by the RCOG Women’s Network and by the RCOG Women’s Voices Involvement Panel.
