This information is for you if you want to know more about pelvic inflammatory disease (PID), how it is diagnosed and how it is treated.
It may also be helpful if you are a relative or friend of someone who has this condition.
Within this information we may use the terms ‘woman’ and ‘women’. However, it is not only people who identify as women who may need to access this information. Your care should be personalised, inclusive and sensitive to your needs whatever your gender identity.
A glossary of medical terms is available at A-Z of medical terms.
Key points
- Pelvic inflammatory disease (PID) is an inflammation of the pelvic organs.
- Diagnosis is usually based on symptoms, examination and test results.
- PID is usually treated successfully with antibiotics. Rarely, surgical treatment may be required.
- You should avoid having any sexual contact until you have completed the course of treatment and follow-up.
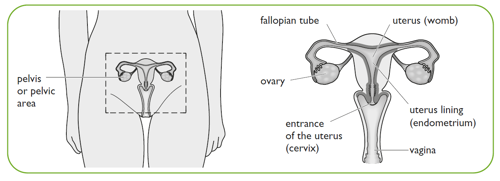
Pelvic Inflammatory disease (PID) is inflammation of the pelvic organs. It is usually caused by an infection spreading from the vagina and cervix to the uterus (womb), fallopian tubes, ovaries and pelvic area. If severe, it can cause an abscess (collection of pus) inside the pelvis.
1 in 4 cases of PID are caused by untreated sexually transmitted infections (STIs) such as chlamydia or gonorrhoea. PID is more common in young sexually active women. PID may also be caused by less common infections that may be sexually transmitted.
Sometimes, PID can happen after:
- a miscarriage
- an abortion,
- having a baby
- having a procedure to the inside of the womb such as hysteroscopy or insertion of a contraceptive device (coil).
Sometimes you may not have any symptoms. You may have one or more of the following, which can vary from mild to severe:
- smelly or unusual vaginal discharge
- pain in the lower abdomen that is usually on both sides and can feel like period pains
- pain deep inside during or after sex
- vaginal bleeding in between periods, bleeding after sex
- nausea and vomiting
- fever
- low backache.
Many of these symptoms are common and can be caused by other conditions.
This means that PID can be difficult to diagnose so, if you have any of these symptoms, it is important to seek medical advice.
Your healthcare professional will ask you about your symptoms and your medical and sexual history. With your consent, your healthcare professional may also do a vaginal (internal) examination. You should be offered a female chaperone for this. The examination may cause some discomfort, especially if you do have PID.
Swabs may be taken from your vagina and your cervix to test for infection. It usually takes a few days for the results to come back.
- a positive swab result confirms that you do have an infection
- a negative swab result means you are less likely to have an infection. It does not mean you definitely do not have an infection.
You may be offered blood tests to check for infection. You may be asked for a urine sample. A test for HIV may also be advised.
If there is a chance that you could be pregnant, you will be offered a pregnancy test. This is because other conditions such as ectopic pregnancy (when a pregnancy develops outside the uterus (womb)) can cause similar symptoms to PID.
If your healthcare professional suspects you have a severe infection, you will be referred to your local hospital for further tests and treatment. You may be offered an ultrasound scan. This is usually a transvaginal scan (where a probe is gently inserted into your vagina) to look more closely at the uterus (womb), fallopian tubes and ovaries. This may help to detect an abscess or other causes for your symptoms.
Your healthcare professional can give you information about the specific treatment you are offered; this should include information about possible side effects.
You will usually be given an injection of an antibiotic followed by a 2 week course of antibiotic tablets. Treatment usually does not affect contraception or pregnancy. It is very important to complete your course of antibiotics even if you are feeling better. Most women who complete the course have no long-term health or fertility problems.
You may also be offered medication for pain relief. You should rest until your symptoms improve. If they get worse, or do not get better within 48 to 72 hours of treatment, you should see your healthcare professional again.
If you have a severe infection, or the antibiotic treatment is not improving the infection you may need to have any abscess drained. This might be done with an operation under general anaesthetic, or by insertion of a drainage tube into the abscess. (See the RCOG patient information Laparoscopy, which is available at: www.rcog.org.uk/en/patients/patient-leaflets/laparoscopy.)
You should start taking antibiotics as soon as they are prescribed, even if you have not had your test results back. This is because any delay could increase the chance of long-term health problems.
Your healthcare professional may recommend treatment in hospital if:
- your diagnosis is unclear
- you are very unwell
- they suspect an abscess in your fallopian tube and/or ovary
- you are pregnant
- you are not getting better within a few days of starting antibiotic tablets
- you are unable to take antibiotic tablets.
When you are in hospital, antibiotics may be given intravenously (directly into the bloodstream through a drip). This treatment is usually continued until 24 hours after your symptoms have improved. After that, you will also be given a course of antibiotic tablets.
You will usually only need an operation if you have a severe infection or an abscess in the fallopian tube and/or ovary. An abscess may be drained during a laparoscopy or during an ultrasound procedure. Your healthcare professional will discuss these treatments with you in more detail.
It is rare to develop PID when you are pregnant. You will be prescribed antibiotics that are safest in pregnancy.
The risks associated with antibiotic treatment for PID are low for both you and your baby. Untreated or undertreated PID does increase the risk of harm to you and your baby.
Your healthcare professional will discuss your options if you have PID during the early stage of pregnancy. You will be supported in your choice of choosing to continue with the pregnancy, or to arrange an abortion.
If your symptoms of PID are not improving within a few days of starting treatment and you have an IUD, your healthcare professional may recommend that you have it removed.
If you have had sex in the 7 days before it is removed, your healthcare professional may recommend the morning-after pill (emergency hormonal contraception). This is because there may be chance of an unplanned pregnancy.
If you have developed PID as a result of an STI, anyone you have had sex with in the last 6 months should be tested for infection, even if they are well. You can contact them yourself or, your healthcare professional, local genitourinary medicine (GUM) clinic or sexual health clinic may help you with this.
You should avoid having any sexual contact until you and have completed the course of treatment, to avoid reinfection.
If you have a moderate to severe infection, you will usually be given an appointment to return to the clinic after 3 days. It is important to attend this appointment so that your healthcare professional can see that your symptoms are responding to the antibiotics.
If your symptoms are not improving, you may be advised to attend hospital for further investigations and treatment.
If your symptoms are improving, you will usually be given a further follow-up appointment 2-4 weeks later to check:
- that your treatment has been effective
- whether a repeat swab test is needed to confirm that the infection has been successfully treated; this is particularly important if you have ongoing symptoms
- that you have all the information you need about the long-term effects of PID
- whether another pregnancy test is needed
- that you have all the information you need about future contraceptive choices
- that your sexual partner(s) have been treated.
Treatment with antibiotics is usually successful for PID. Long-term problems can arise if it is untreated, if treatment is delayed, or if there is a severe infection.
The long-term effects can include:
- an increased risk of ectopic pregnancy in the future
- difficulties in becoming pregnant
- an abscess in a fallopian tube and/or ovary
- persistent pain in your lower abdomen; see the RCOG patient information Chronic (long-term) pelvic pain.
Repeated episodes of PID increase the risk of you having future fertility problems, developing long term pelvic pain, or needing to have surgery. Risks of further infection can be reduced by using condoms and by making sure that you and your sexual partner(s) have been treated.
Further information
Sources and acknowledgements
This information has been developed by the RCOG Patient Information Committee. It is based on the British Association for Sexual Health and HIV (BASHH) 2019 publication UK National Guideline for the Management of Pelvic Inflammatory Disease.
Published November 2016; updated January 2026
Please note that this information will be reviewed every 3 years after publication.
