This information is for you if you have been told that you have a thyroid problem or if you have been offered testing for thyroid problems and you are pregnant or planning a pregnancy.
It may also be helpful if you are a partner, friend or relative of someone who is in this situation.
The information here aims to help you better understand your health and your options for treatment and care. Your healthcare team is there to support you in making decisions that are right for you. They can help by discussing your situation with you and answering your questions.
Within this information we may use the terms ‘woman’ and ‘women’. However, it is not only people who identify as women who may want to access this leaflet. Your care should be personalised, inclusive and sensitive to your needs whatever your gender identity.
You can read a glossary of all medical terms.
Key points
- Thyroid problems are common in women.
- Hypothyroidism is when your body does not make enough thyroid hormones. This can be safely treated with levothyroxine tablets.
- Hyperthyroidism is when your body makes too much of the thyroid hormones. Treatment will depend on the underlying cause, but during pregnancy this usually involves taking anti-thyroid tablets.
- Untreated thyroid problems may cause complications in pregnancy and can affect your baby’s health.
- If your thyroid problems is well treated, you are highly likely to have an uncomplicated pregnancy and to give birth to a healthy baby.
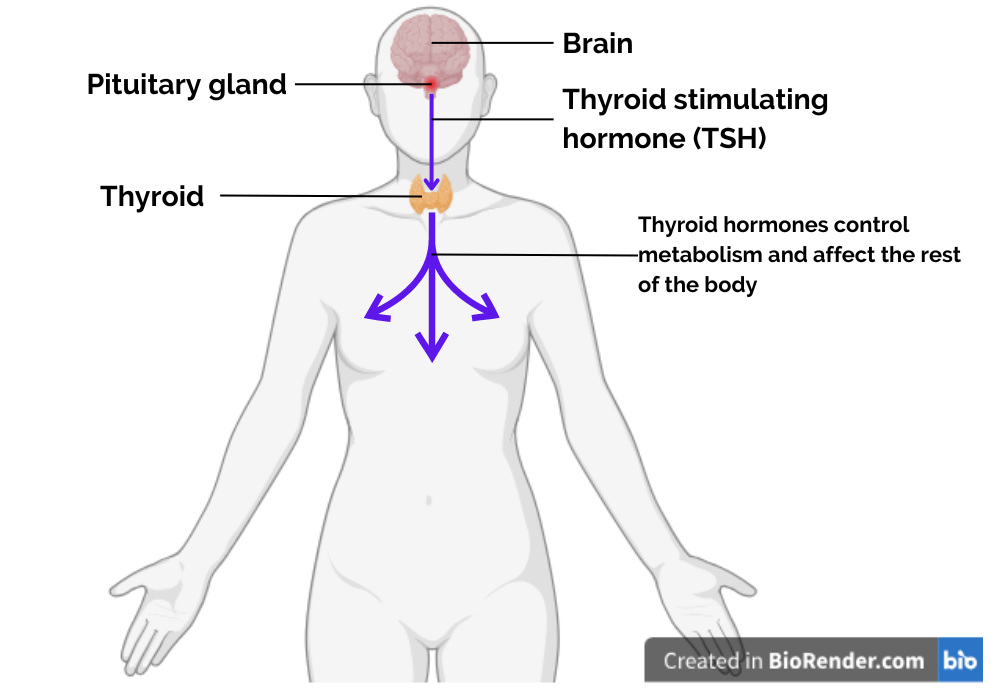
The thyroid gland is a butterfly shaped gland located in the front of your neck.
It makes hormones (commonly called thyroxine) which control your metabolism and affect different organs including your heart, muscles and brain.
A second hormone called Thyroid Stimulating Hormone (TSH), helps your thyroid gland make thyroxine. TSH is made by the pituitary gland in your brain.
When you are pregnant, your body usually makes more thyroxine for both you and your baby.
You may get thyroid problems if you do not have enough iodine in your diet. This is more important if you are pregnant, planning a pregnancy or breastfeeding.
Sources of iodine include:
- cow’s milk
- yoghurt
- eggs
- fish such as cod or haddock.
Iodine is sometimes added to table salt and is found in some pregnancy multivitamins.
The recommended daily amount of iodine when planning a pregnancy, while you are pregnant and whilst breastfeeding is 200-250 micrograms. If you think you may not have enough iodine in your diet, for example if you follow a vegan diet, speak to your healthcare professional about whether iodine supplements may be helpful for you.
It is recommended to start taking pregnancy vitamin supplements 3 months before you become pregnant if possible. Iodine (150 micrograms) is found in common multivitamins you can buy. It is important not to take too much iodine as this can be harmful to you and your baby, so you should avoid taking multiple different vitamin supplements.
Sometimes thyroid problems are caused by an autoimmune condition. This is where your own immune system attacks different organs in your body. Your healthcare professional will arrange a blood test for this type of problem if needed.
You will be offered a blood test in early pregnancy (first trimester) to check your thyroid function if:
- you have had thyroid problems in the past
- you have had an operation on your thyroid gland
- you have a swelling in your thyroid gland
- you have another autoimmune disease such as Type 1 diabetes, systemic lupus erythematosus or antiphospholipid syndrome.
You will also be offered a thyroid blood test if you have had a stillborn baby or late miscarriage and have not had the test before.
Hypothyroidism is when your body does not make enough thyroxine. It is sometimes called having an underactive thyroid.
Symptoms of hypothyroidism may include:
- tiredness
- increased awareness of cold
- dry skin and hair
- constipation
- heavy or irregular periods or fertility problems.
Hypothyroidism is confirmed by a blood test to check your thyroid function.
Sometimes, you may have normal thyroxine levels but a high TSH level (subclinical hypothyroidism). Your healthcare professional will discuss with you as to whether this needs treatment or not.
If your hypothyroidism is well treated it will not cause any harm to you or your baby.
Untreated hypothyroidism during pregnancy may be linked with a higher chance of:
- Miscarriage
- Premature birth
- Your baby having a low birthweight
- Your baby’s brain development being affected.
Hypothyroidism is treated using a tablet called Levothyroxine, which is safe to take during pregnancy.
When you are pregnant, your body needs more thyroxine than usual. If you are already taking Levothyroxine tablets before becoming pregnant, your healthcare professional will discuss changing your dose when you become pregnant.
If you are diagnosed with hypothyroidism or severe sub clinical hypothyroidism during pregnancy, you will be started on levothyroxine as soon as possible.
You will be offered thyroid blood tests at your first appointment with your midwife and regularly throughout pregnancy to make sure you are on the right dose of Levothyroxine.
Having well controlled hypothyroidism will not change how or when you give birth. Your healthcare professional will support you in making a birth plan that is right for you.
Once your baby is born you can go back onto the dose of Levothyroxine you were taking before you became pregnant. If you were not on levothyroxine before becoming pregnant, you may be able to stop taking it all together.
Your thyroid blood tests should be checked again when your baby is 6 weeks old to make sure you are on the correct treatment.
Hyperthyroidism is when your body makes too much thyroxine. It is sometimes called having an overactive thyroid.
The most common cause for hyperthyroidism is Grave’s disease. This is an autoimmune condition where there are thyroid antibodies in your blood that cause the thyroid gland to make more thyroxine than it needs to.
Symptoms of hyperthyroidism include:
- weight loss
- heart palpitations
- intolerance to heat
- shakiness
- mood swings
- enlarged thyroid gland
- very prominent eyes.
Hyperthyroidism is diagnosed by a blood test to check your thyroid function.
If your hyperthyroidism is well treated, there is low chance of any harm to you or your baby. It is important to make sure that your hyperthyroidism is well controlled before becoming pregnant.
Poorly controlled hyperthyroidism during pregnancy may be linked with a higher risk of:
- Pre-eclampsia (See RCOG patient information Pre-eclampsia)
- Premature birth
- Your baby having a low birthweight
- Stillbirth
Your baby may also have a higher chance of having additional learning needs, autism or ADHD (attention deficit hyperactivity disorder).
If you have Grave’s disease and have high thyroid antibody levels there is a chance of your baby getting hyperthyroidism before or soon after they are born. In this situation, your baby will be monitored more closely before and after birth.
Hyperthyroidism during pregnancy is usually treated with anti-thyroid tablets, such as propylthiouracil or carbimazole. Some of these tablets are safer for your baby’s development than others. The lowest possible dose of anti-thyroid tablets will be advised.
If you are planning to become pregnant, your healthcare professional will discuss your treatment options with you.
If you become pregnant unexpectedly while taking anti-thyroid tablets, you should tell your health care professional straight away so that a personalised plan of care can be made.
Your healthcare professional will offer you regular blood tests in pregnancy to check your thyroid function and your thyroid antibody levels. The type and the dose of your medication may change depending on your blood tests. Your healthcare professional may also offer you regular scans to check your baby’s growth.
If your hyperthyroidism is well controlled, it should not affect how or when you give birth and your healthcare professional will support you in making a birth plan that is right for you.
You will usually be advised to give birth in the labour ward with your baby’s heartbeat checked continuously during labour if:
- You have Grave’s disease
- You have high thyroid antibodies
- You have been taking anti-thyroid medication during pregnancy.
You will be offered blood tests 6 weeks after giving birth to check your hormone levels.
Your baby will also have thyroid blood tests taken soon after birth and again when they are 1-2 weeks old if:
- You have Grave’s disease
- You have high thyroid antibodies
- You have been taking anti-thyroid medication during pregnancy.
Medications to treat hypothyroidism or hyperthyroidism are safe to take while breastfeeding.
If you are on anti-thyroid medication for hyperthyroidism your health care team will support you to take the lowest safe dose for you, so that the amount of the medication that passes into your breast milk is as low as possible.
You will be supported in however you choose to feed your baby.
Gestational transient thyrotoxicosis
This type of hyperthyroidism happens in the first half of pregnancy, when the level of the pregnancy hormone hCG is high. This sometimes causes the thyroid gland make more thyroxine than it needs to.
This condition usually settles by itself and does not affect your pregnancy or your baby’s health. The treatment depends on your symptoms and you are unlikely to need to take anti-thyroid tablets.
Thyroid nodules and Thyroid cancer
Swelling in a part of the thyroid gland is called a thyroid nodule. Most thyroid nodules are harmless and do not need treatment. If you notice a swelling on your neck during pregnancy, you should tell your healthcare professional. You may be referred to a specialist for further assessment and treatment.
You may also be referred to an anaesthetist who will make sure the nodule is not affecting your breathing. Rarely, you may need a biopsy of the thyroid gland to rule out cancer. Thyroid cancer developing during pregnancy is very rare, happening in less than 1 case in 10,000 births.
Postpartum thyroiditis
This is an autoimmune inflammation of your thyroid gland. It can happen in the 12 months after you have given birth.
You should have your thyroid function checked if you have symptoms of:
- Hyperthyroidism
- hypothyroidism or
- severe postnatal depression.
Sometimes you may not have any symptoms.
Postpartum thyroiditis is more common if you have other autoimmune conditions or a family history of thyroid problems.
Treatment depends on your symptoms and you may not need anti-thyroid tablets. Postpartum thyroiditis usually gets better by itself, but you might develop hypothyroidism in the future. You should have your thyroid function checked every year and at the start of any future pregnancies.
Emotional support
Having any medical condition while you are pregnant can be stressful. If you are feeling anxious or worried in any way, please speak to your healthcare team who can answer your questions and help you get support. The support may come from healthcare professionals, voluntary organisations or other services. Further information and resources are available on the NHS website.
Further information
- British Thyroid foundation
- British Thyroid foundarion: Pregnancy and Fertility disorders in Thyroid
- The UK Iodine group
Making a choice

Sources and acknowledgements
This information has been developed by the RCOG Patient Information Committee. It is based on the RCOG guideline Management of Thyroid Disorders in Pregnancy (Published April 2025). The guideline contains a full list of the sources of evidence we have used.
Published December 2025
This resource will be reviewed every 3 years after publication.
