Published: March 2013
Please note that this information will be reviewed every 3 years after publication.
This information is for you if you wish to know about shoulder dystocia. You may also find it helpful if the birth of your baby was complicated by shoulder dystocia.
It may be helpful if you are a partner, relative or friend of someone who has been in this situation.
The information here aims to help you better understand your health and your options for treatment and care. Your healthcare team is there to support you in making decisions that are right for you. They can help by discussing your situation with you and answering your questions.
This information covers:
- What shoulder dystocia is, and how commonly it occurs
- Whether shoulder dystocia can be predicted or prevented
- What happens if shoulder dystocia occurs
- What happens if you give birth at home or in a midwife-led unit
- What happens if you’ve chosen to have a water birth
- What shoulder dystocia could mean for you and your baby
- Implications for future deliveries
Within this information, we may use the terms ‘woman’ and ‘women’. However, it is not only people who identify as women who may want to access this information. Your care should be personalised, inclusive and sensitive to your needs, whatever your gender identity.
A glossary of medical terms is available at A-Z of medical terms.
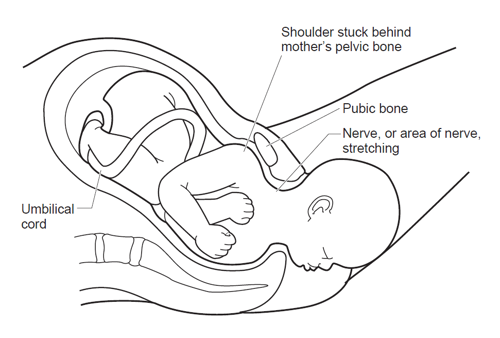
Shoulder dystocia is when the baby’s head has been born but one of the shoulders becomes stuck behind the mother’s pubic bone, delaying the birth of the baby’s body (see figure below). If this happens, extra help is usually needed to release the baby’s shoulder. In the majority of cases, the baby will be born promptly and safely.
Shoulder dystocia occurs in about one in 150 (0.7%) vaginal births.
Shoulder dystocia usually occurs unexpectedly during childbirth and most of the time it is not possible to predict when it will happen. However, it is more likely to occur if:
- you have had shoulder dystocia before
- you have diabetes
- your body mass index (BMI) is 30 or more
- your labour is induced
- you have a long labour
- you have an assisted vaginal birth (forceps or ventouse).
Shoulder dystocia is more likely with large babies but nevertheless there is no difficulty delivering the shoulders in the majority of babies over 4.5 kg (10 lb). Half of all instances of shoulder dystocia occur in babies weighing less than 4 kg (about 9 lb).
Ultrasound scans are not good at telling whether you are likely to have a large baby and therefore they are not recommended for predicting shoulder dystocia, if you have no other risk factors
In most instances, shoulder dystocia cannot be prevented because it cannot be predicted.
If you have diabetes or have developed diabetes in pregnancy, you will usually be offered early induction of labour or planned caesarean section. This will reduce the risk of shoulder dystocia.
If you don’t have diabetes, early induction of labour does not prevent shoulder dystocia, even if your baby is suspected to be large. Caesarean section is also not routinely recommended in this situation.
Your midwife and obstetrician will be aware that in every birth there is a possibility of shoulder dystocia.
Shoulder dystocia is an emergency and therefore, when it does occur, speed is of the essence. The baby’s shoulder needs to be released quickly so that the baby’s body can be born and he or she can start breathing air into the lungs. Your midwife will push the emergency bell and three or four members of staff, including obstetricians, midwives and a doctor for the baby (paediatrician), are likely to come into the delivery room to help.
Because it happens so quickly and lots of people come into the room, it may be frightening for you and your birth partner. However, it is important to remember that obstetricians and midwives who attend the birth are trained in how to release the shoulders using certain manoeuvres and in the great majority of cases your baby will be delivered promptly and safely.
The obstetrician or midwife will usually:
- ask you to stop pushing
- reposition you to give your baby more room inside the vagina; you will be asked to lie on your back with your legs pushed outwards and up towards your chest (this is known as the McRoberts manoeuvre)
- press on your abdomen just above the pubic bone to try to release your baby’s shoulder
- consider making a cut (episiotomy) to enlarge the vaginal opening.
With these simple measures, the majority of babies are born safely.
If the shoulder is not released easily with the above measures, either:
- your obstetrician or midwife will put his or her hand within the vagina to try to free your baby’s shoulder, or
- you may be helped to roll over onto ‘all fours’, which can also help to release the shoulder.
Once the shoulders are free, your baby will be born, and a paediatrician will examine him or her. Your midwife and obstetrician will talk to you about what happened. If you wish to talk at a later date about your experience, ask to talk to your obstetrician, midwife, health visitor and/or GP.
Wherever you give birth, your midwife is trained to deal with shoulder dystocia. If your baby is not born with the simple measures described above or by rolling over onto all fours, your midwife will call an ambulance to transfer you to hospital. If your baby is born before the ambulance arrives, your midwife may still suggest taking you and your baby to hospital to be checked over.
If you are having a water birth, you will be asked to get out of the pool so that your midwife can assist you.
For me
Vaginal tears are more common after shoulder dystocia and may extend to the back passage (see RCOG patient information: Care of a third- or fourth-degree tear that occurred during childbirth (OASI)). Heavier bleeding than normal after birth (postpartum haemorrhage) is also more common and you may require additional treatment and/or a blood transfusion.
For my baby
About one in ten (10%) babies who have shoulder dystocia will have some stretching of the nerves in the neck (see figure on page 1), called brachial plexus injury (BPI), which may cause loss of movement to the arm. The most common type of BPI is called Erb’s palsy. It is usually temporary and movement will return within hours or days. Permanent damage is rare.
It is important to remember that BPI can occur without shoulder dystocia. BPI can also occur in babies born by caesarean section.
Sometimes shoulder dystocia can cause other injuries including fractures of the baby’s arm or shoulder. In the majority of cases, these heal extremely well.
Even with the best care, in a very few cases, a baby can suffer brain damage if he or she did not get enough oxygen because the delivery was delayed by shoulder dystocia.
If your baby’s birth was complicated by shoulder dystocia, there is an increased risk of shoulder dystocia in future pregnancies; around one in ten women will have shoulder dystocia again in a future pregnancy. In view of this, your obstetrician or midwife will discuss your options for next time taking into account your individual circumstances and preferences.
You may wish to consider a vaginal delivery if it was easy to release your baby’s shoulders, your baby was fine and you have no other risk factors. If it was difficult to release your baby’s shoulders, your baby had any injuries or the experience has affected you and your family, you may wish to consider a planned caesarean section.
If you are asked to make a choice, you may have lots of questions that you want to ask. You may also want to talk over your options with your family or friends. It can help to write a list of the questions you want answered and take it to your appointment.
Ask 3 Questions
To begin with, try to make sure you get the answers to 3 key questions, if you are asked to make a choice about your healthcare:
- What are my options?
- What are the pros and cons of each option for me?
- How do I get support to help me make a decision that is right for me?
*Ask 3 Questions is based on Shepherd et al. Three questions that patients can ask to improve the quality of information physicians give about treatment options: A cross-over trial. Patient Education and Counselling, 2011;84:379-85
Sources and acknowledgements
This information is based on the RCOG guideline Shoulder Dystocia (March 2012). The guideline contains a full list of the sources of evidence we have used
This information has been reviewed before publication by women attending clinics in Cambridge, Poole and London.
