What are perineal tears?
Your perineum is the area between your vaginal opening and back passage (anus). It is common for the perineum to tear to some extent during childbirth. Tears can also occur inside the vagina or other parts of the vulva, including the labia. Up to nine in every 10 first time mothers who have a vaginal birth will experience some sort of tear, graze or cut (episiotomy). It is slightly less common for mothers who have had a vaginal birth before.
For most women, these tears are minor and heal quickly. They are very unlikely to cause long-term problems, but they can be very sore. For more information on tears, please visit the RCOG Tears Hub.
What is an OASI?
For some women, a tear may be deeper and extend to the muscle that controls the anus (the anal sphincter).
Third- or fourth-degree tears, also known as an obstetric anal sphincter injury (OASI) or severe tears, can occur in 6 out of 100 births (6%) for first time mothers and less than 2 in 100 births (2%) for women who have had a vaginal birth before.
A rectal buttonhole is a rare injury that occurs when the anal sphincter does not tear, but there is a hole between the back passage and the vagina.
Although most women or birthing people who sustain an OASI recover well, it may take longer than a less severe tear. Occasionally, long-term pain and a difficulty or inability to control the bladder, bowels or the passing of wind can occur. Please contact your doctor or midwife for specialist care if you experience this.
For more information on ways to reduce your risk and recovering from an OASI, please visit the RCOG Tears Hub.
What is a care bundle?
The US Institute for Healthcare Improvement (IHI) originally developed care bundles to describe a collection of interventions needed to care safely for patients. They define a care bundle as a small set of evidence-based interventions for a defined patient segment or population and care setting which, when implemented together, will result in significantly better outcomes than when implemented individually.
What is the OASI Care Bundle?
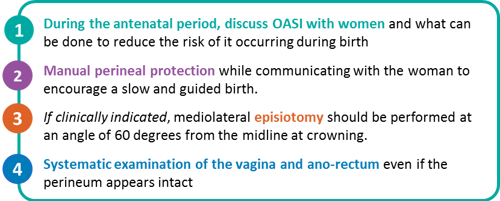
The OASI Care Bundle consists of four practices that should be used together to reduce the risk of severe perineal tearing:
Why is it important that all four components of the OASI Care Bundle are used?
A care bundle is a small set of evidence-based interventions that, when implemented together, will result in better outcomes than when implemented individually. It is therefore ideal to apply all four elements of the care bundle to an eligible birth.
Supporting women’s informed choice and decision-making autonomy is a priority, and therefore all components of the OASI Care Bundle are individually subject to the woman’s informed consent. All components of the OASI Care Bundle should be discussed with the woman during antenatal care so that she is supported to give informed consent and choose which practices are a part of her birth plan.
How was the OASI Care Bundle developed and who was involved?
In 2014, the RCOG and the RCM convened a working group of expert obstetricians, midwives and methodologists to address the impact of OASI. The working group reviewed national and international initiatives to reduce perineal trauma and agreed on developing a care bundle of interventions. The working group, along with a lay member of the RCOG Women’s Network, then convened to reviewed evidence from national guidelines, randomised controlled trials (RCTs) and key observational studies of intrapartum care interventions to reduce OASI. The academic research databases used in this review included EMBASE, Ovid MEDLINE, the Cochrane Library, the Maternity and Infant Care database and CINAHL.
The themes identified in the review included: episiotomy, perineal protection, maternal position, pushing technique and coaching, instrument choice and “other” (which included pain relief, water birth, hyaluronidase and use of devices such as EpiScissors). Overview of the evidence highlighted that most RCTs that reported OASI outcomes lacked sufficient statistical power to evaluate the intervention’s impact on OASI rates, and meta-analyses of RCTs within each theme were difficult to interpret owing to significant heterogeneity in the definition of the interventions included.
The OASI Care Bundle components were selected following consideration of various definitions of interventions, the quality of evidence, as well as the feasibility for their inclusion into a standardised care bundle. The OASI Care Bundle was further refined following an RCM consultation with labour ward specialists, managers and educationalists, which resulted in an emphasis on clinicians’ engagement with women, mobility during labour and facilitating chosen birth positions.
Patient and public involvement was incorporated in the development of the OASI Care Bundle and throughout the OASI1 and OASI2 projects, with both projects supported by an Independent Advisory Group that included two lay representatives. The antenatal discussion guide (designed to support the first component of the OASI Care Bundle) was developed together with women’s groups to ensure that the content was appropriate, whereas lay representatives were present at all skills development days for clinicians.
How does the OASI Care Bundle differ from other projects such as PEACHES?
The PEACHES programme was initially developed at St Thomas' Hospital in London in 2015. PEACHES stands for:
P = Position
E = Extra midwife (present at birth)
A = Assess the perineum (throughout)
C = Communication
H = Hands-on technique
E = Episiotomy if required
S = S-L-O-W-L-Y
There are similarities between PEACHES and the OASI Care Bundle. The differences are that the OASI Care Bundle recommends an extra midwife at birth but does not require it. The position, assessment, communication and ‘slowly’ elements are incorporated into the OASI Care Bundle rather than being individual elements. Finally, the OASI Care Bundle places emphasis on diagnosis, through the systematic examination of the vagina and ano-rectum.
Where has the OASI Care Bundle been used and what impact has it had?
The OASI1 project focused on evaluating the clinical effectiveness of the OASI Care Bundle in reducing OASI rates. Funded by the Health Foundation, OASI1 was implemented in 16 maternity units across England, Scotland and Wales from January 2017 to April 2018. Project results were published in the BJOG, BMJ Open and IUJ journals and are available to download from the OASI1 webpage.
The OASI1 project evaluated 55,060 live singleton vaginal births across the 16 participating maternity units and showed that through adoption of the care bundle, overall OASI rates were reduced from 3.3% before the project started to 3.0% upon its conclusion. There was shown to be no rise in caesarean section or episiotomy rates through use of the care bundle. Using data modelling that takes into account case mix factors such as age, ethnicity and body mass index, women’s estimated risk of sustaining an OASI was reduced by 20% in maternity units where the OASI Care Bundle was introduced.
What is the OASI2 project and how is it different to the first OASI Care Bundle project?
After the OASI1 project established the care bundle’s clinical effectiveness and broad acceptability to women and clinicians, the project team was awarded additional funding from the Health Foundation to scale-up the initiative in more maternity units. This second project, “OASI2”, ran from September 2021 to December 2022. It took place in 10 of the original sites that participated in OASI1 in addition to 19 newly recruited maternity units. OASI2 aimed to evaluate the implementation of the care bundle in new maternity units with different levels of external support, while continuing to achieve further reductions in OASI rates in a way that is acceptable to women giving birth. For more information, please visit the OASI2 webpage.
Does the care bundle work?
The care bundle was initially piloted in two units and then rolled out to 16 maternity units as part of OASI1. The end-of-project evaluation showed that women’s risk of sustaining an OASI reduced by 20% if giving birth in a unit that had implemented the care bundle, without changing rates of caesarean births or episiotomy. Furthermore, the interviews and focus groups undertaken as part of the evaluation demonstrated that the OASI Care Bundle was both acceptable and feasible to women and clinicians. You can read the full results of the OASI1 evaluation by downloading the open access articles published by BJOG, BMJ Open and IUJ.
Will the care bundle affect birth choices?
No. The OASI Care Bundle respects and supports women’s choices about how they wish to give birth. The first element of the care bundle ensures clinicians understand the importance of discussing women’s birth choices so she is well informed about all practices that may reduce her risk of sustaining a severe tear. The antenatal discussion guide encourages discussing perineal massage, birth environment, movement during labour, birth positions, use of warm compress, when an episiotomy might be recommended, and manual perineal protection. Informed decision-making requires that these discussions include the risks and benefits of birth choices in an unbiased and balanced way so women can make the decisions that are right for them.
The OASI Care Bundle does not prescribe a woman’s position for birth, nor does it recommend restricting her movement during birth. The aim is to prevent and diagnose perineal trauma. Clinicians should use evidence to support and advise women about their choice of birth position. The care bundle interventions can be used with women in most positions. Ultimately, the choice is always the woman’s, armed with the best available information and support.
How were women involved in the OASI1 and OASI2 projects?
Women were at the heart of both the OASI1 and OASI2 projects. Women have been involved in discussions and decision-making around the care bundle including in the design, governance and steering of the OASI1 and OASI2 projects. Both projects’ Independent Advisory Group (IAG) membership included women with lived experience of OASI who informed and inputted into all project developments. The IAG had further representation from women’s advocacy organisations including the Birth Trauma Association the MASIC Foundation, while the Project Team also sought advice and input from members of the RCOG Women’s Network.
