About this information
This information is for you if you are pregnant or planning a pregnancy and want information about COVID-19 infection.
This information will cover:
- COVID-19 and pregnancy
- How to protect yourself and your baby from COVID-19.
For more information about COVID-19 vaccines, see the accompanying Fact Sheet: COVID-19 Vaccines and pregnancy.
This information may also be helpful if you are a partner, relative or friend of someone who is in this situation.
The information here aims to help you better understand your health and your options for treatment and care. Your healthcare team is there to support you in making decisions that are right for you. They can help by discussing your situation with you and answering your questions.
Within this information we may use the terms ‘woman’ and ‘women’. However, we know that it is not only people who identify as women who may want to access this information. Your care should be appropriate, inclusive and sensitive to your needs whatever your gender identity.
A glossary of all medical terms is available on the RCOG website
Key points
- COVID-19 is a virus which usually causes cold or flu-like symptoms. It can sometimes cause severe illness, mostly in people who have not been vaccinated, or have other health conditions.
- Most women who get COVID-19 during pregnancy will recover without complications and will go on to have a healthy baby.
- Some pregnant women who get COVID-19 can have a life-threatening illness, particularly if they have other health conditions.
- In the later stages of pregnancy, women who are unvaccinated and get COVID-19 have a higher chance of becoming seriously unwell or dying from it than people who are not pregnant.
- If you are unvaccinated and get COVID-19 while you are pregnant, your baby has a higher chance of being born prematurely or dying before birth.
- COVID-19 vaccination is the safest and most effective way of protecting you and your baby from COVID-19 infection.
- Pregnant women are strongly advised to take up the offer of COVID-19 vaccination when this is recommended.
COVID-19 is a viral infection that was first identified towards the end of 2019. It is usually spread through close contact with an infected person.
Most pregnant women are no more likely to get COVID-19 than other healthy adults.
Some pregnant women do have an increased risk of catching the virus, for example if you have diabetes or are overweight (Body Mass Index over 25).
Many women do not experience symptoms when infected with COVID-19. Symptoms you may experience include:
- high temperature (fever),
- shivering (chills)
- a new continuous cough
- loss of taste and/or smell
- shortness of breath
- tiredness and muscle aches
- headache
- sore throat
- blocked or runny nose
- loss of appetite and diarrhoea.
More severe infection can cause pneumonia and serious complications including life-threatening breathing difficulty, sepsis, blood clots, heart problems and death.
To confirm a diagnosis of COVID-19, you will need to take a test. This can be done at home, or at the hospital. For the most up to date information on testing, see the NHS information on testing for COVID or contact your healthcare professional.
Most pregnant women who test positive for COVID-19 have no symptoms or only a mild cold or flu-like illness.
- You may have a higher chance of severe infection if you:
• have high blood pressure,
• have diabetes,
• are overweight (Body Mass Index over 25),
• are older than 35,
• have another medical condition,
• are from a minority ethnic group,
• live in an area of social disadvantage.
If you have COVID-19 infection in pregnancy, you are more likely to develop severe illness and need hospital care, compared to someone who is not pregnant. The risk of severe infection is highest in women who get COVID-19 in the last three months of pregnancy (after 28 weeks).You are more likely to need care in an Intensive Care Unit.
You are also more likely to need an emergency caesarean birth compared to a pregnant woman without COVID-19.
What about ‘Long COVID’?
At present, it is not known whether pregnancy has any effect on the chance of developing ‘long COVID’ after having had COVID-19 infection.
If you have COVID-19 during pregnancy:
- Your baby does not have a higher chance of having a problem with their physical development (congenital anomaly.
- Your baby may not grow as well as they should, especially if you have other conditions which can affect your baby’s growth. If you have had COVID-19, you may be offered extra scans during pregnancy to monitor your baby’s growth.
- Your chance of stillbirth (your baby dying before birth) is increased from up to 5 per thousand to around 10 per thousand compared to a woman who does not have COVID-19 during pregnancy. This is not always related to how severe your COVID-19 infection is. However, stillbirth is still a rare event.
- You may have a higher chance of a late miscarriage (after 20 weeks).
- Your baby has a higher chance of being born early (prematurely). This is usually because your healthcare professionals recommend that your baby needs to be born to help with your treatment. Babies who are born prematurely may have a range of health problems, which tend to be more serious the earlier they are born.
If you have COVID-19 during pregnancy or at the time you give birth, the chance of your baby catching the virus is very low. It is safe for you to have skin-to-skin contact with your baby after they are born. Even if your baby does catch COVID-19 infection soon after birth, they usually remain well.
The most effective way to protect yourself is to be vaccinated.
- Vaccination dramatically reduces your chance of needing hospital admission and developing severe infection.
Being vaccinated against COVID-19 will: - Reduce your chance of having COVID-19 infection.
- Reduce your chance of having severe infection which requires admission to hospital.
- Reduce your chance of having very severe infection needing intensive care. Almost all pregnant women who are admitted to intensive care units have not been vaccinated.
- Protect your baby from catching COVID-19 and needing admission to hospital with COVID-19 in the first 6 months of their life.
There are also simple things you can do in your daily life that will help reduce the spread of COVID-19 and other respiratory infections:
- Let fresh air in if meeting others indoors.
- Practise good hygiene:
• wash your hands
• cover your coughs and sneezes
• clean your surroundings frequently
• Think about wearing a face covering if you are in close contact with other people or in crowded places.
If you work, your employer is required to carry out a pregnancy risk assessment for you as an individual to ensure your working environment is safe for you.
If you think you might have COVID-19 you need to follow the current NHS advice which applies to everyone.
Try to stay at home and avoid contact with other people. Take extra care to avoid close contact with anyone who is at higher risk of getting seriously ill from COVID-19.
Speak to your healthcare professional or maternity team – they will advise you what to do.
If you have mild symptoms, you will be advised to stay at home. To look after yourself at home, try to keep well hydrated and mobile. You may be advised to have treatment to prevent you getting blood clots if you are at higher risk of this. Your maternity team will assess your risk and arrange this if needed.
You can go back to your normal activities when you feel better.
If you feel your symptoms are worsening or if you are not getting better, this may be a sign that you are developing a more severe infection that requires hospital admission and specialised care. You should contact your maternity team, GP, or use the NHS 111 online service (or NHS 24 in Scotland) for further information and advice. In an emergency, call 999.
Seek medical advice as early as possible if you have any questions or concerns about you or your baby. This advice is important for all pregnant women, but particularly if you are at higher risk of becoming seriously unwell.
It is important that you still attend your appointments and scans. If you have an appointment scheduled, tell your maternity unit that you think you have COVID-19 before attending. Your appointment may be rearranged or carried out by phone or video. If you have a scan appointment, depending on the reason for the scan, it may be rearranged, or you may need to attend at a different time to reduce contact with others.
- Oxygen
- Steroids
- Help with your breathing, which in severe illness, can mean admission to the intensive care unit for extra support.
- Specific medications and antibody treatment.
- A caesarean birth may be recommended if you or your baby are unwell or there are other complications. However, your chance of needing an emergency caesarean birth may be higher than usual.
- All the usual options for pain relief for labour and birth are available to you, however a water birth is not recommended. This is because it is harder to monitor and give you any treatments needed.
- Wash your hands.
- Try to avoid coughing or sneezing on your baby.
- Consider wearing a mask or face covering while feeding.
Emotional support
Further information
- GOV.UK.
- COVID-19 Symptoms and what to do
- How to avoid catching and spreading COVID-19.
- Reducing the spread of respiratory infections, including COVID-19, in the workplace.
Best use of medicines in pregnancy (bumps) COVID-19 Vaccinations. - COVID-19 vaccination: women who are pregnant or breastfeeding.
- COVID-19 vaccines.
- Long COVID.
- Vitamins, supplements and nutrition in pregnancy.
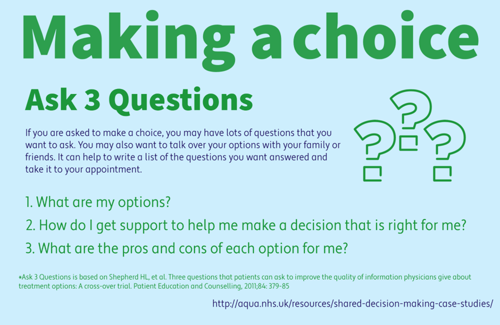
Making a Choice
Sources and acknowledgements
COVID-19 Vaccine Fact Sheet
COVID-19 vaccination is strongly recommended for all women who are planning to become pregnant, having fertility treatment, or are pregnant to protect them and their baby from the effects of COVID-19 infection.
Vaccination Facts:
- COVID-19 vaccination is considered safe for you and can be given at any time before, during and after pregnancy.
- COVID-19 vaccination is considered safe for your baby.
- Worldwide data looking at many thousands of women vaccinated in pregnancy has shown no increased risk of miscarriage, stillbirth, premature birth or problems with baby’s development or growth.
- COVID-19 vaccination does not cause infertility in women or men.
- There is no need to delay getting pregnant after being vaccinated.
- You should complete the course of vaccination according to the usual schedule, including booster doses, and not delay because you are pregnant.
- Vaccination is most effective if the course including the booster dose is completed before the last three months of pregnancy (before 28 weeks).
- The vaccines approved for use in the UK are all safe in pregnancy, but certain vaccines are currently recommended as there is more information about these (Pfizer-BioNTech and Moderna).
- The vaccine cannot cause COVID-19 infection in you or your baby, as they are not ‘live’ vaccines. ‘Live’ vaccines are not used in pregnancy due to the risk of causing infection.
- Influenza (‘flu’) and whooping cough vaccinations (both non-live vaccines) are also recommended and can be given at the same time as COVID-19 vaccine.
- You can safely breastfeed your baby if you have been vaccinated.
Any vaccine may have a chance of side effects or complications. The chance of having complications from the COVID-19 vaccine is very small and does not increase if you have the vaccine while you are pregnant.
The decision whether to have any vaccination in pregnancy is your choice. Make sure you understand as much as you can about COVID-19 and vaccination. You may want to discuss your options with your health care professional.
