This information is for you if you have been told you may have endometriosis.
It may also be helpful if you are a partner, friend or relative of someone who is in this situation.
The information here aims to help you better understand your health and your options for treatment and care. Your healthcare team is there to support you in making decisions that are right for you. They can help by discussing your situation with you and answering your questions.
Within this information, we may use the terms ‘woman’ and ‘women’. However, it is not only people who identify as women who may want to access this information. Your care should be personalised, inclusive and sensitive to your needs, whatever your gender identity.
A glossary of medical terms is available at A-Z of medical terms.
Key points
- Endometriosis occurs when tissue similar to the inner lining of your uterus (womb) is found elsewhere in your body, usually in your pelvis around your uterus, ovaries and fallopian tubes.
- Endometriosis is not always straightforward to diagnose, as there is no blood test, it does not always show up on scans, and symptoms overlap with other conditions.
- Common symptoms include pelvic pain and painful periods. It may cause pain during or after sex, affect your bowel or bladder, or may lead to fertility problems.
- Treatment options include pain-relieving medications, hormones and/or surgery.
The lining of your uterus is called your endometrium.
Endometriosis is when cells similar to the cells from your endometrium are found growing elsewhere, usually in the pelvis.
It is a common condition, affecting up to 10 in 100 women. You are more likely to develop endometriosis if your mother or sister has had it.
Endometriosis can affect women at any age from puberty to menopause. It is a long-term condition that can have an impact on your general physical health, emotional wellbeing and daily routine.
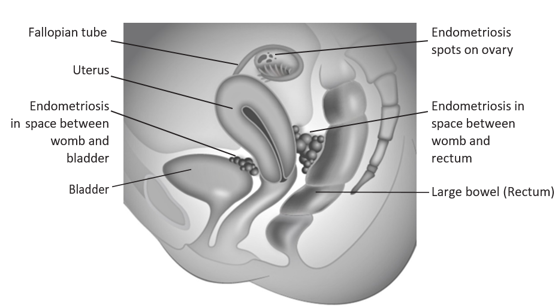
Endometriosis can be found:
- on the peritoneum (the lining of the pelvis and abdomen),
- on the ovaries where it can form cysts (often referred to as 'chocolate cysts' or endometriomas),
- on, or around the uterus
- on, or within the fallopian tubes
- in the area between the vagina, the bladder or the bowel.
Endometriosis may sometimes be found in other parts of the body including scars following surgery, the belly button and the chest, but these are less common.
The exact cause of endometriosis is not known. There are a number of theories but none of these have been proven. It is likely that there are several reasons why some women develop endometriosis and others do not.
Further information on possible causes of endometriosis can be found on the Endometriosis UK website: www.endometriosis-uk.org/causes.
Symptoms of endometriosis vary between women. Your symptoms will depend on where your endometriosis is, and some may have no symptoms at all.
Common symptoms can include:
- pelvic pain which may change throughout your menstrual cycle,
- very painful periods,
- pain when you open your bowels or pass urine, which is often worse during your period,
- bleeding from your bowels or bladder during your period,
- pain during or after sex,
- difficulty in getting pregnant,
- fatigue.
Sometimes, the symptoms can be similar to pain caused by other conditions such as irritable bowel syndrome (IBS) or pelvic inflammatory disease (PID) (see RCOG patient information Acute pelvic inflammatory disease (PID): tests and treatments, and RCOG patient information Long term pelvic pain).
Your healthcare professional will ask about your symptoms in detail.
They may carry out an internal examination with your consent. This helps to find where the pelvic pain is and allows the doctor to feel for any lumps or tender areas. You will be offered a chaperone during this examination. You will be able to discuss any concerns and you will have an opportunity to ask other questions.
Depending on your symptoms, you may be offered the following investigations:
- A transvaginal (internal) ultrasound scan – this may show whether there are any cysts on your ovaries or may show other evidence of endometriosis in your pelvis.
- An MRI scan – this can be useful if you have more extensive endometriosis including involvement of your bowel or bladder.
- Laparoscopy – this is keyhole surgery and is carried out under a general anaesthetic. It can be used to diagnose and to treat endometriosis. You may be offered this surgery if initial treatment to help your symptoms is not effective.
A normal result from an ultrasound or MRI scan does not rule out endometriosis, however it will help guide suitable treatment options.
The treatment of endometriosis depends on a variety of factors, including:
- the type and severity of your symptoms,
- how much endometriosis you have, and where it is,
- whether you are planning a pregnancy,
- whether you wish to use contraception,
- your personal preferences for treatment.
You may be offered a combination of medical, hormonal and surgical treatment.
If you have extensive endometriosis, for example on your bowel or bladder, you should be referred to an endometriosis specialist service. You will be able to discuss your treatment options with a specialist team, which could include a gynaecologist, a nurse specialist, a bowel surgeon, a bladder surgeon and specialists in pain management.
Pain-relieving medication
There are several different medications that may treat your pain.
Some medications relieve pain while others may help to reduce inflammation caused by endometriosis.
Medications can range from over-the-counter treatments (such as paracetamol and ibuprofen) to medications prescribed by your healthcare professional.
In situations where initial treatments have not been helpful, you may be referred to a specialist pain management team that may include physiotherapists and psychologists.
Hormone treatments
Hormone treatments can help control your symptoms. Hormone treatments can reduce bleeding and inflammation from your endometriosis and reduce pain by stopping your periods. If you are prescribed hormone treatment, it is recommended that you give it at least 3–6 months to work.
Most hormone treatments that may be offered are contraceptive so will stop you becoming pregnant while you are having treatment. They do not affect your fertility in the longer term. Hormone treatments include:
- The combined oral contraceptive pill or patch given continuously without the normal pill-free break; this usually stops ovulation and aims to temporarily stop your periods or makes them lighter and less painful.
- A progestogen releasing intrauterine device, which aims to reduce the pain and make periods lighter; some women using this get no periods at all.
- Progestogens in the form of an injection, the mini pill or the contraceptive implant.
If these hormonal methods do not improve your symptoms, there are additional hormonal treatments that your healthcare professional may discuss with you, depending on your individual circumstances and preferences. This includes gonadotropin-releasing hormone (GnRH) agonists, which are injections designed
to temporarily stop your ovaries from producing estrogen and progesterone hormones. This causes a temporary menopause, with similar symptoms to when someone’s periods come to an end naturally. GnRH agonists may be used in the short term to suppress your pain or to suppress inflammation caused by endometriosis in preparation for surgery. Hormone replacement medication is usually given alongside a GnRH agonist to reduce some of the menopause-related side effects.
If you experience side effects as a result of hormonal treatments or if you choose not to use these treatments, your healthcare professional will discuss alternative options with you.
For further information on hormone treatments for endometriosis, see the NICE Patient Decision Aid: Hormone treatment for endometriosis symptoms - what are my options?
Surgery
The type of surgery you may be offered for endometriosis will depend on your individual situation. Success rates vary and you may need further operations. Your gynaecologist will discuss the different types of surgery with you, including the risks and benefits, to support you to make an informed choice.
Most women can be treated by laparoscopic (keyhole) surgery. Small cuts are made in your abdomen and a small camera called a laparoscope is inserted to look at your pelvis. This is used to see the areas of endometriosis. Surgical instruments are inserted through other cuts, and in combination with the laparoscope, endometriosis in your abdomen or cysts on your ovaries can be treated. A laparoscopy includes a vaginal examination and can involve inserting an instrument into your uterus (womb). This allows the uterus to be positioned during the laparoscopy to get the best views of your pelvis. In some situations a rectal examination may also be needed to help get a better view of the pelvis.
Surgery for extensive or deep endometriosis can be more complex. This is usually done in specialist centres, with support from bladder and bowel specialists.
Depending on your circumstances, sometimes a hysterectomy with or without removal of the ovaries can be considered. This will not necessarily cure your endometriosis, but may help with other symptoms.
For information about recovery following a laparoscopy, please see the RCOG patient information Laparoscopy – recovering well.
Fertility treatment
While many women with endometriosis will be able to conceive naturally, for some endometriosis means it can take longer or be more difficult to get pregnant. If you are having difficulties becoming pregnant, your healthcare professional will provide you with information about your options and may refer you to a fertility
specialist for further investigations and treatment if needed. The treatment you may need and the options available to you will depend on your individual circumstances.
Being told you may have endometriosis, and living with endometriosis can be very stressful. If you are feeling anxious or worried in any way, please speak to your healthcare team who can answer your questions and help you get support. The support may come from healthcare professionals, voluntary organisations or other services.
Physical examinations
The nature of gynaecological and obstetric care means that physical examinations are often necessary. This may involve an examination of your abdomen or an internal examination of your vagina.
We understand that for some women, including those who have experienced trauma, physical or sexual abuse, such examinations can be very difficult. Your healthcare professionals are there to provide kind and personalised care to you. If you choose not to be examined, they can discuss alternative options with you.
After explaining to you about the physical examination you are being offered, your healthcare professional will seek your consent. You should always be offered a chaperone. This could be a partner, family member, friend, support person or another healthcare professional.
If you feel uncomfortable, anxious, distressed or in pain at any time before, during, or after an examination, please let your healthcare professionals know, as they are there to support you.
If you find this difficult to talk about, you may communicate your feelings in writing or with the support of someone you wish to accompany you.
You can ask your healthcare professional to stop at any time during your physical examination.
Further information
- Endometriosis UK
- The Endometriosis Foundation
- NHS information on Endometriosis
- NHS Inform (Scotland)
- Endometriosis Cymru
- Fertility Network UK
- British Society for Gynaecological Endoscopy
RCOG Recovering Well series:
If you are asked to make a choice, you may have lots of questions that you want to ask. You may also want to talk over your options with your family or friends. It can help to write a list of the questions you want answered and take it to your appointment.
Ask 3 Questions
To begin with, try to make sure you get the answers to 3 key questions, if you are asked to make a choice about your healthcare:
- What are my options?
- What are the pros and cons of each option for me?
- How do I get support to help me make a decision that is right for me?
*Ask 3 Questions is based on Shepherd et al. Three questions that patients can ask to improve the quality of information physicians give about treatment options: A cross-over trial. Patient Education and Counselling, 2011;84:379-85
Sources and acknowledgements
This information has been developed by the RCOG Patient Information Committee and Endometriosis UK. It is based on the NICE guidelines and ESHRE guidelines. Further information can be obtained from:
National Institute of Health and Care Excellence (NICE): Endometriosis: Diagnosis and Management.
European Society of Human Reproduction and Embryology (ESHRE): Endometriosis.
