A multiple pregnancy means you are having more than one baby at the same time. This is most commonly twins, but may includes triplets, or, rarely, more.
This information is for you if you are having a multiple pregnancy. It may also be helpful for your partner, family or friends.
It focuses on twin and triplet pregnancies. If you are having more babies you can still use this information but you will have an individualised plan of care for your pregnancy depending on your circumstances.
The information here aims to help you better understand your health and your options for treatment and care. Your healthcare team is there to support you in making decisions that are right for you. They can help by discussing your situation with you and answering your questions.
This information tells you about:
- the different types of multiple pregnancy
- what it means for you and your babies
- the care you will receive while you are pregnant
- the options for birth so that you can make an informed choice
- where to find further advice and support
Within this information, we may use the terms ‘woman’ and ‘women’. However, it is not only people who identify as women who may want to access this information. Your care should be personalised, inclusive and sensitive to your needs, whatever your gender identity.
A glossary of medical terms is available at A-Z of medical terms.
Key points
- Multiple pregnancy happens in about one in 60 pregnancies.
- Most women with multiple pregnancies will have a healthy pregnancy and will give birth to healthy babies, however complications are more common.
- You will be offered extra antenatal checks and ultrasound scans to make sure that you are well and to monitor your babies closely.
- If you have a multiple pregnancy you are more likely to give birth to your babies prematurely
- You will be advised to give birth in hospital.
A multiple pregnancy is the term used when you are expecting two or more babies at the same time (twins, triplets or more). It happens in about one in 60 pregnancies. Multiple pregnancy is more common as you get older or if you have fertility treatment.
Twins or triplets can be identical (monozygotic) or non-identical (di/tri-zygotic).
Identical twins or triplets have come from one egg, which has been fertilised by one sperm and has then split into two (or three) after fertilisation. Identical twins or triplets share identical genes, will look the same and be the same sex.
Non-identical twins or triplets have come from different eggs, which have been fertilised by different sperm. If your babies are non-identical, they will have different genes and will be no more similar than any other brothers or sisters.
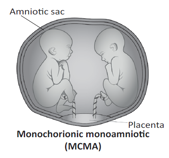
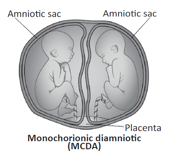
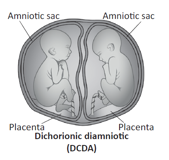
Chorionicity refers to whether your babies each have their own placenta or whether they share a placenta. If your babies share a placenta (monochorionic) they are always identical. If they each have their own placenta (dichorionic/trichorionic) they are more likely to be non-identical but can still be identical.
Chorionicity is checked for at your first ultrasound scan. It is important to know about this because babies who share a placenta have a higher chance of having complications during the pregnancy.
Your first ultrasound scan also checks whether each baby is within their own amniotic sac or whether they share a sac. Babies who share a sac also have a higher chance of complications. Twins can be:
- Dichorionic Diamniotic (DCDA) – This means each baby has its own placenta and its
- own sac.This is the most common type of twin pregnancy.
- Monochorionic Diamniotic (MCDA) – This means the babies share a placenta but they are each in their own sacs.
- Monochorionic Monoamniotic (MCMA) – This means that both babies share a placenta and are within the same sac.This is a much rarer type of twin pregnancy.
Similarly, triplets can be trichorionic (each baby has a separate placenta), dichorionic (two of the three babies share a placenta and the third baby has its own placenta), or monochorionic (all three babies share a placenta).
 |
 |
 |
Most women who are having twins or triplets have a healthy pregnancy and will give birth to healthy babies. However, complications are more common and you will be offered extra care during your pregnancy.
Problems that many pregnant women experience, such as morning sickness, heartburn, swollen ankles, varicose veins, backache and tiredness, are all more common in multiple pregnancies.These will get better after you have given birth but ask your healthcare professional if you are worried about any of these symptoms.
Additionally, you are more likely than someone having a single baby to experience more serious problems during your pregnancy.This may include:
- Anaemia – this is usually caused by a shortage of iron because your developing babies use up a lot of iron.You will be offered regular blood tests to check whether you are becoming anaemic and you will be offered treatment with tablets if your iron levels are low. For further information see RCOG patient information Healthy eating and vitamin supplements in pregnancy.
- Pre-eclampsia – this is a condition that causes high blood pressure and protein in your urine during pregnancy.Your blood pressure and urine will be checked regularly and, depending on your other risk factors, you may be advised to take aspirin tablets to reduce your chance of developing this. For further information, see the RCOG patient information Pre-eclampsia.
- A higher chance of needing a caesarean birth or an assisted vaginal birth (forceps or ventouse) - your healthcare team will support you to create a birth plan and you should discuss your choices and preferences with your team. For further information see the RCOG patient information Assisted Vaginal Birth.
- Post-partum haemorrhage – this means that you may bleed more than average after you have given birth.You will be offered medications at birth to reduce the chance of this happening. For further information see the RCOG patient information Heavy bleeding after birth (postpartum haemorrhage).
Prematurity
Overall around 8 in 100 babies (8%) are born prematurely (before 37 weeks).This is more common if you have a multiple pregnancy and can either be because you go into labour early or because your healthcare team recommend that the babies are born early.
If you are pregnant with twins you have a 60 in 100 (60%) chance of going into labour and giving birth before 37 weeks of pregnancy.
If you are pregnant with triplets you have a 75 in 100 (75%) chance of going into labour and giving birth before 35 weeks.
Babies born prematurely have an increased chance of health problems, particularly with breathing, feeding and infection. The earlier your babies are born, the more likely this is to be the case.
Depending on how early they have been born, they might need to spend time in the neonatal unit. Wherever possible your babies will be kept together however depending on their individual needs they may need to be cared for separately.
Problems with growth
Having a multiple pregnancy increases the chance that your placenta may not work as well as it should. This can affect the babies’ growth and wellbeing during the pregnancy. Sometimes both babies may be small but more often only one baby is small. If only one baby is affected this is called selective fetal growth restriction (S-FGR).
You will be offered extra ultrasound scans during your pregnancy to check for growth problems:
- if you are having DCDA twins you will be offered scans at least every 4 weeks from 24 weeks.
- if you are having MCDA or MCMA twins you will be offered scans at least every 2 weeks from 16 weeks.
- if you are having triplets or more you will be offered growth scans depending on your specific circumstances.
Twin-to-twin transfusion syndrome (TTTS)
Babies who share a placenta (monochorionic pregnancies) also share the blood supply from the placenta. In around 15 in 100 (15%) monochorionic pregnancies, the blood flow to the babies may be unbalanced. This is called twin-to-twin transfusion syndrome (TTTS).Triplet pregnancies can also be affected by this. One baby, the ‘donor’, receives too little blood while the other baby, the ‘recipient’, receives too much blood. It can be mild and may not require any treatment, or it can be serious, in which case you will be offered treatment in a hospital with specialist expertise. You will be monitored with frequent scans for signs of TTTS.
If you notice any of the following you should contact your healthcare professional immediately:
- sudden abdominal pain and/or swelling
- sudden breathlessness
- change in the babies’ movements.
You will be under the care of a specialist healthcare team throughout your pregnancy. This should include a doctor, a midwife and a sonographer who specialise in multiple pregnancies. You will be offered additional support as you need it from other team members, which may include dieticians, physiotherapists, mental health specialists, health visitors and infant feeding specialists. You will have an individualised plan of care for your pregnancy and birth that will include additional visits to the antenatal clinic and extra growth scans for the babies. You should be given information about what to expect from having a multiple pregnancy and a detailed plan of care at your first appointment with your specialist team. This should be by the time you are around 16 weeks pregnant. Sometimes referral to a specialised fetal medicine unit, which may be in a different hospital, may be recommended.
For further information, see Twins Trust: https://twinstrust.org/let-us-help/pregnancy-and-birth/ preparing-for-birth/antenatal-care/care-pathway.html.
Like all women, you will be offered screening for chromosomal conditions, such as Down’s syndrome, at about 12–14 weeks. However, this is less accurate for multiple pregnancies. Should the result of the screening test show that there is an increased chance of a baby with a chromosomal condition it can be difficult to know which baby is affected. In this situation, you will be offered further specialist counselling and information from your health care team. If you would like further support to help you decide whether to have screening, please speak to your healthcare professional.
General information about these conditions and the screening tests available can be found in the UK National Screening Committee’s (UK NSC) information booklet Screening tests for you and your baby.
You will also be offered another scan at around 20 weeks to look at your babies’ development. The chance of these tests finding a genetic or structural condition is slightly higher than if you were pregnant with only one baby.Your specialist team will be able to offer you information and advice if the screening shows a higher chance of a genetic or structural condition.
You will be advised to give birth in hospital with midwifery and medical support.This may be at your local hospital or at a more specialist unit depending on how your pregnancy has been and whether or not you have gone into labour early.
The exact timing of birth in a multiple pregnancy will depend on your individual circumstances; however, even if your pregnancy has been uncomplicated, you should be offered a planned birth before your due date.This is because it has been found to be safer for your babies than continuing with the pregnancy to full term.The recommended timing of birth is usually:
- Around 37 weeks of pregnancy if you are having DCDA twins
- Around 36 weeks if you are having MCDA twins
- Around 32–34 weeks if you are having MCMA twins
- Around 35 weeks if you are having triplets.
Your health care team should start to discuss your birth plan with you from around 24 weeks. Your decision as to whether to plan for a vaginal birth (usually after an induction of labour) or a caesarean birth will depend on several factors including the position in which the babies are lying in your uterus (womb), how well the babies are growing and your personal preferences about the birth.
Twins
Both vaginal birth and caesarean birth have benefits and risks, which will depend on your individual circumstances.Your healthcare professional should discuss these with you to enable you to make an informed choice.
If the baby lying nearest to your cervix (the neck of the womb) is head-down and you have no other complications, then you should be able to plan for a vaginal birth if you choose.The position of the second twin can change after the first baby is born and should not influence how you choose to give birth. More than a third of women having twins who plan a vaginal birth will go on to need a caesarean birth.
If the baby nearest to your cervix is bottom-down (breech) towards the end of the pregnancy, a caesarean birth is usually recommended.
If you have planned to have a caesarean but go into labour naturally before the date of your operation, you should go straight to hospital.Your healthcare team will advise whether the safest option for you is to go ahead with your caesarean as planned or to give birth vaginally.This will depend on the situation at the time.
Monoamniotic twins and triplets
These babies are usually born by caesarean unless you are in very premature labour.Your own birth preferences are important and you will have time to discuss these with your healthcare team.
During labour extra measures will be recommended to look after you and your babies. You will be offered:
a cannula (a small tube) in your hand to give you fluids and medication if needed.
an epidural for pain relief while you are in labour. As well as providing good pain relief an epidural may also be helpful if your babies need to be born quickly by caesarean or by assisted vaginal birth. All options for pain relief should be discussed with you while you are pregnant and again when you are in labour. For further information on pain relief in labour see information from the Obstetric Anaethetists’ Association: www.labourpains.com.
continuous monitoring of your babies’ heartbeats using a machine called a CTG.This helps to show how your babies are coping during labour; however it may make it less easy for you to move around.Your first baby’s heartbeat may be monitored by applying a tiny clip to their head, via your vagina.
The room may seem crowded when your babies are being born.There will usually be two midwives present. An obstetrician will be in the room or close at hand. Doctors and nurses specialising in the care of newborn babies may also be present.
After your first baby is born, the cord will be clamped and cut but the placenta will stay inside your uterus until your second baby has been born.
Your healthcare team will check whether your second baby is coming head-first or bottom-first by feeling your abdomen, doing an internal examination and by carrying out an ultrasound scan. The second baby is usually born within about 30 minutes to an hour of the birth of the first baby.
In a small number of cases you may need a caesarean for the birth of the second baby after the first baby has been born vaginally.This is only done if becomes unsafe for your second baby to be born vaginally.
After both your babies and their placenta have been born you will be offered medication to minimise the risk of having heavy bleeding (postpartum haemorrhage). See RCOG patient information on Heavy bleeding after birth (postpartum haemorrhage). If you do have heavy bleeding there is a chance that you may need a blood transfusion. If you think that you could never accept a blood transfusion, discuss this with your healthcare team as early as possible in your pregnancy. For further information see RCOG patient information on Blood transfusion, pregnancy and birth.
You should be offered advice about feeding your babies during your pregnancy and support with feeding after they are born. How you choose to feed your babies is a very personal decision. There are many benefits of breastfeeding for you and your babies but feeding more than one baby can be challenging. Extra help is available if you need it from your healthcare team and local support organisations.You can find further information from the Twins Trust.
You may want to consider colostrum harvesting (expressing breast milk while you are pregnant so you have some milk ready to give your babies when they are born). For further information see Association of Breastfeeding Mothers.
Like anyone who has given birth you will have routine visits from your healthcare team when you get home. Having a multiple pregnancy and giving birth to more than one baby can be challenging. Having as much help and support as possible makes it easier and you may want to plan this well ahead. Activities and support groups are available for families having multiple pregnancies (see below).
Support is especially important if you have had complications in your pregnancy or if your babies have needed to go to a neonatal unit.
Your emotional wellbeing is also very important and you may experience anxiety or have low mood. If you feel that you need additional support you should talk to your healthcare professional. You can find further information from the Maternal Mental Health Alliance or Twins Trust.
The nature of obstetrics and gynaecology care means that intimate examinations are often necessary.
We understand that for some people, particularly those who may have anxiety or who have experienced trauma, physical abuse or sexual abuse, such examinations can be very difficult.
If you feel uncomfortable, anxious or distressed at any time before, during or after an examination, please let your healthcare professional know.
If you find this difficult to talk about, you may communicate your feelings in writing.
Your healthcare professionals are there to help and they can offer alternative options and support for you.
Remember that you can always ask them to stop at any time and that you are entitled to ask for a chaperone to be present.You can also bring a friend or relative if you wish.
Further information
- Twins Trust
- Twins Trust support line called Twinline: 0800 138 0509 asktwinline@twinstrust.org
- NHS information on twin pregnancies
- Multiple Births Foundation
- National Institute for Health and Care Excellence (NICE) guideline: Twin and triplet pregnancy
- RCOG Green-top Guideline Management of Monochorionic Twin Pregnancy
- NHS Fetal Anomaly Screening Programme
- Maternal Mental Health Alliance
- Tommy’s
- Bliss
Sources and acknowledgements
This information has been developed by the RCOG Patient Information Committee. It is based on the NICE clinical guideline Twin and triplet pregnancy (published in 2019) and the RCOG Green-top Guideline Management of monochorionic twin pregnancy (published in 2016).
The guidelines contain full lists of the sources of evidence used.
Before publication this information was reviewed by the public and by representatives from the RCOG Women’s Network and the RCOG Women’s Voices Involvement Panel.
