Effective clinical escalation requires clear, succinct communication with the right person at the right time.
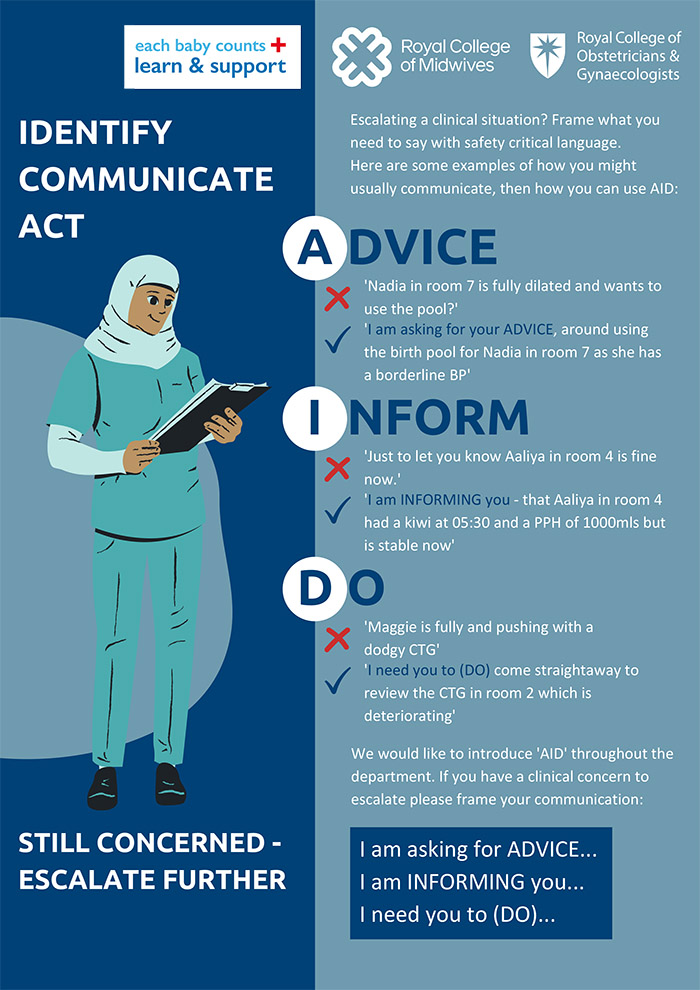
It also requires receiving the correct response at the right time, often in a complicated, evolving clinical situation. The overall the aim of this intervention is to improve time critical escalation in order to reduce delays in the process, and identify when clinical escalation is taking place. AID is as a clear and simple communication tool which initiates escalation conversations using 3 simple phrases:
“I am asking you for Advice”,
“I am Informing you” and
“I need you to Do…”
It is designed to precede the commonly used SBAR (situation, background, response) which is a tool used to describe the clinical situation.
It can also be used “in reverse” – ie if it is unclear what response the person escalating is looking for, the clinician being escalated to can ask the following:
“Are you asking me for Advice”,
“Are you Informing me”,
“Do you need me to DO something / what would you like me to DO”?
It is not expected that clinicians force these exact phrases into conversations, but that the principles of “ADVICE, INFORM, DO” are used as a framework when escalating.
What does AID aim to do?
- Clearly identify when escalation is taking place
- Elicit a time critical response, reducing delays
- Help prioritisation for clinicians who may receive multiple escalations within any given shift (band 7 midwifery co-ordinators, consultants)
- Empower junior staff
When is AID used?
- At the outset of all escalation conversations between ALL members of the MDT
- Particularly helpful when escalating to non resident clinicians (usually consultants) and during periods of high activity
What did clinicians say about AID?
- Simple, empowering, works as a safety net – therefore well received, particularly by the people being escalated to.
- Streamlines communication and creates escalation awareness
- Improves responses and decision making
- Improves communication and teamwork
- Flattens hierarchies
What are the potential barriers?
- Concerns that it replaces SBAR (it is designed to precede it)
- Some people are resistant to using acronyms or changing engrained practice
- Some junior staff were worried that it might come across as rude to their seniors – in fact it was most well received by seniors and those being escalated to
Key implementation strategies
- Send introductory emails, place posters around the unit, hand out business cards and other merchandise (eg pens)
- Discuss it at all handovers, huddles until embedded
- Use your shop floor champions – and engage the early adopters
- Be prepared to receive feedback – acknowledge that change can be hard
- Use it in training sessions – particularly CTG / intrapartum care teaching
- Disseminate it to the whole MDT so that it becomes normalised practice in your unit
- Celebrate successes